M.Anurag
8th semester
Roll number: 72
I have been given the following cases to solve in an attmept to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and coem up with a treatment plan.This is the link of the questions asked regarding the cases
This is the link of the questions asked regarding the cases :
Below are my answers to the Medicine Assignment based on my comprehension of the cases.
1) PULMONOLOGY:
A) A 55 year old female patient, with the chief complaints of shortness of breath, pedal edema and facial puffiness.
Patient details: https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-female-with-shortness-of.html
QUESTIONS :
1. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANSWER:
a)Symptomatology in this patient:
20 years back:
-Shortness of breath on and off for the past 20 years
-1st episode lasted for a week while she was working in a paddy field
-Relieved on taking medication.
-For the next 8 years the patient has suffered from similar episodes of SOB every year each lasting aproximately 1 week and occurring around January (when she worked at the paddy fields) these episodes were all relieved upon taking medication.
↓
12 years back:
-Developed an episode Oscar shortness of breath in the moth of January while working in paddy feild
-Lasted for about 20 days for which she had to be hospitalised
-Relieved after hospitalisation
-For the past 12 years she has been having an yearly episodes now lasting around a month again around january. Until her latest episode the SOB was of grade II
↓
1 month back:
-Latest episode of SOB which wand insidious in onset and gradual in progression
-It was occurring on exertion and was getting relieved on taking rest(Grade 2)
↓
20 days back:
-She got a HRCT done due to the ongoing COVID-19 pandemic which showed signs of bronchectiasis
-She was diagnosed to be hypertensive 20 days ago and was treated for the same.
-She experienced generalised weakness for which she was administered IV fluids by the local RMP
↓
15 days back:
-Pedal edema( level: ankle, pitting type)
-Facial puffiness
↓
2 days back:
-Shortness of breath(grade 4 which did not get received even after using nebulisers)
-Drowsiness
-The patient was also diagnosed for diabetes 8 years and treated for the same ; diagnosed for iron deficiency anemia and awash treated for the same.
b) Anantomical localisation:
The lesions of the disease are localised to the entire lung bilaterally and also generalised honey comb lesions are present in the lungs
c) Primary etiology:
The primary etiology is the periodic working in the paddy fields and being exposed to various types of environmental pollutants and also certain organisms such as various bacteria, viruses and fungi.
The patient also uses indoor chulka which increases the chances for COPD due to improper ventilation.
2. What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANSWER:
Head end elevation:
Mechanism of action:
Head of bed elevation (HOBE) is a commonly used therapeutic intervention in mechanically ventilated patients associated with a reduction in the incidence of ventilator-associated pneumonia. HOBE has also been shown to improve oxygenation and hemodynamic performance
Efficacy over placebo:
A change in the angle of the head affects the respiratory mechanics of MV patients. In this study, the largest resistive pressure value was found at the 0º position, and the largest value of elastic pressure was found at the 60º position.
A comparison of the 35 evaluated patients revealed that the resistive airway pressure values in the 0° position were higher than those obtained when patients were positioned at greater angles. The elastic pressure analysis revealed that the 60° position produced the highest value relative to the other positions. Regarding static compliance, a reduction in values was observed from the 0° position to the 60° position. The dynamic compliance analysis revealed that the 30° angle produced the greatest value compared to the other positions. The peripheral oxygen saturation showed little variation, with the highest value obtained at the 0° position.
Indication:
- Patients presenting with decreased oxygen saturation and requiring mechanical saturation
- Children presenting with head trauma
- Patients with acute cerebral infections that such as meningitis
- Patients having conditions which increase intracranial pressure
O2 inhalation:
Mechanism of action:
Oxygen therapy is prescribed for people who can't get enough oxygen on their own. This is often because of lung conditions that prevents the lungs from absorbing oxygen, including: chronic obstructive pulmonary disease (COPD) pneumonia
Efficacy over placebo:
Evidence of enhanced survival benefit with supplemental oxygen is provided by the National Institutes of Health. The study assessed whether continuous supplemental oxygen improved survival compared with nocturnal oxygen. Eligible subjects had COPD and severe resting hypoxemia (Pao2 ≤ 55 mm Hg or Pao2 ≤ 59 mm Hg with either edema, polycythemia [hematocrit, ≥ 55%], or P pulmonale on electrocardiogram). The study enrolled 203 subjects. Over a mean follow-up period of 19.3 months, use of continuous oxygen conferred a significant survival benefit (P = .01), with a relative risk of death of 1.94 (95% CI, 1.17-3.24) with use of nocturnal oxygen compared with continuous oxygen. Among secondary outcome measures, hematocrit fell more in continuous than in nocturnal oxygen users (P = .008 at 18 months), and pulmonary vascular resistance fell 11.1% in continuous oxygen users but rose 6.5% in nocturnal oxygen users (P = .04 at 6 months). Subjects receiving continuous oxygen therapy averaged (mean ± SD) 17.7 ± 4.8 h/d, and subjects receiving nocturnal oxygen therapy averaged 12.0 ± 2.5 h/d.
Results of the NOTT demonstrated that use of continuous supplemental oxygen enhanced survival compared with use of nocturnal supplemental oxygen. Taken together with the results of the MRC study, the findings suggest that in patients with COPD and resting hypoxemia, some oxygen is better than none, and continuous oxygen is better than nocturnal oxygen.
Indications:
-Hypoxemia / hypoxia
-Respiratory distress
-Increased metabolic demand (burns, multiple injuries, severe sepsis)
-Cardiac failure or myocardial infarction
-Short term therapy (post anesthesia recovery)
Intermittent BiPAP:
Mechanism of action :
BiPAP acts through expiratory positive airway pressure. During the expiratory phase, the noninvasive ventilator lowers airway pressure to a preset EPAP, which is synonymous with the PEEP. This maintains small-airway patency, prevents atelectasis and increases FRC, drastically improving oxygenation.
Efficacy over placebo:
Use of NIV, especially in the early course of the disease, has revolutionized the management of patients with AECOPD. It is clearly a superior alternative to standard medical therapy during the initial phase of management of these patients. NIV should be considered for all the patients unless there is a contraindication to its use. It should be avoided in extremely sick, hemodynamically unstable and obtunded patients, who are better managed by invasive conventional mechanical ventilation. Data on use in markedly hypercapnic or severely acidotic patients is sparse, but future studies may address these issues. All patients initiated on NIV must be closely watched for the initial period as early response tends to predict success of the intervention. NIV is also a viable option for weaning of patients with AECOPD. Again, early rather than late use is associated with better outcomes. Long term nocturnal use of NIV in patients with very severe COPD is useful in improving blood gas parameters, dyspnea and quality of life and may also favorably impact long term survival.
In a systematic review of 21 randomized controlled trials, 3–6 days of oral antibiotics had comparable efficacy with the standard 10 day duration of oral penicillin in treating children with acute GABHS pharyngitis [20]. Clinical efficacy of 3 day azithromycin therapy (95–100%) was similar to 10 day penicillin therapy (95–97%) in a review of management of acute Streptococcal tonsillopharyngitis. Bacteriological eradication was less in azithromycin 10 mg/kg/day groups (38–58%) compared to penicillins (81–84%) whereas azithromycin 20 mg/kg/day therapy achieved bacteriological eradication in 95% cases. Authors suggested that a higher dose of azithromycin was more appropriate for management of acute Streptococcal tonsillopharyngitis [21]. Bacteriological eradication is more important from point of view of preventing progression of pharyngitis to acute rheumatic fever.
Indications:
-Acute or chronic hyper panic respiratory failure
-Decompensated acidosis
-Acute exacerbation of bronchectiasis
-ARDS( post operative, post transplant respiratory)
-Weaning of invasive ventilation
-Heart failure/ Pneumonia
References: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2629986/
Augmentin:
Mechanism of action:
Amoxicillin binds to penicillin-binding proteins within the bacterial cell wall and inhibits bacterial cell wall synthesis. Clavulanic acid is a β-lactam, structurally related to penicillin, that may inactivate certain β-lactamase enzymes.
Efficacy over placebo:
Patients with exacerbations of mild to moderate COPD have a higher rate of cure when given amoxicillin/clavulanate compared with placebo.
"Approximately 75 percent of patients treated with antibiotics were cured, compared with 60 percent of those treated with placebo (number needed to treat = 8; 95% confidence interval, 5 to 27). Additionally, patients taking antibiotics had a longer time to the next exacerbation compared with patients taking placebo (233 versus 160 days)"
Indications:
Antibiotics should only be started or continued in patients with signs and symptoms of a bacterial infection that include the following:
- Increased dyspnea, increased purulence of sputum, and increased volume of sputum.
- Ventilator support (invasive or non-invasive) for AECOPD.
Patients with a PCT <0.1 ng/mL are unlikely to benefit from antibiotic administration.
References :
Azithromycin:
Mechanism of action:
Azithromycin binds to the 23S rRNA of the bacterial 50S ribosomal subunit. It stops bacterial protein synthesis by inhibiting the transpeptidation/translocation step of protein synthesis and by inhibiting the assembly of the 50S ribosomal subunit.
Efficacy over placebo:
In a systematic review of 21 randomized controlled trials, 3–6 days of oral antibiotics had comparable efficacy with the standard 10 day duration of oral penicillin in treating children with acute GABHS pharyngitis [20]. Clinical efficacy of 3 day azithromycin therapy (95–100%) was similar to 10 day penicillin therapy (95–97%) in a review of management of acute Streptococcal tonsillopharyngitis. Bacteriological eradication was less in azithromycin 10 mg/kg/day groups (38–58%) compared to penicillins (81–84%) whereas azithromycin 20 mg/kg/day therapy achieved bacteriological eradication in 95% cases. Authors suggested that a higher dose of azithromycin was more appropriate for management of acute Streptococcal tonsillopharyngitis [21]. Bacteriological eradication is more important from point of view of preventing progression of pharyngitis to acute rheumatic fever.
Indications:
Antibiotics should only be started or continued in patients with signs and symptoms of a bacterial infection that include the following:
- Increased dyspnea, increased purulence of sputum, and increased volume of sputum.
- Ventilator support (invasive or non-invasive) for AECOPD.
Patients with a PCT <0.1 ng/mL are unlikely to benefit from antibiotic administration.
References: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3918299/
Inj Lasix:
Mechanism of action:
Furosemide works by blocking the absorption of sodium, chloride, and water from the filtered fluid in the kidney tubules, causing a profound increase in the output of urine (diuresis).
Efficacy over placebo:
Furosemide decreases peripheral edema and decreases PaCO2 and also increases FEV1 scores when discontinued in patients with COPD as compared to the placebo.
"Ventilation increased from 10.4 L/min (range, 6.7 to 15.4 L/min) at baseline to 11.6 L/min (range, 8.7 to 14.0 L/min) after discontinuation of furosemide (p < 0.05). PaCO(2) decreased from 45 mm Hg (range, 35 to 64 mm Hg) to 41 mm Hg (range, 32 to 61 mm Hg; p < 0.01)"
Indication:
patients with stable COPD who satisfied the following criteria:
- Moderate to severe COPD (FEV1 < 70% predicted) with a clinical course consistent with chronic bronchitis and/or emphysema
- Moderate to severe chronic breathlessness (Medical Research Council Dyspnea Scale Grades 4 and 5)
- Age 50 years or older
References :
Mechanism of action:
Steroids are among the medications commonly prescribed to people with COPD. They help reduce the inflammation in your lungs caused by flare-ups. Steroids come in oral and inhaled forms
Efficacy over placebo:
In comparison to placebo, systemic corticosteroids improve airflow, decrease the rate of treatment failure and risk of relapse, and may improve symptoms and decrease the length of hospital stay.
"Compared with placebo, systemic corticosteroids reduced treatment failure by 46% (95% confidence interval [CI], 0.41 to 0.71), length of hospital stay by 1.4 days (95% CI, 0.7 to 2.2), and improved FEV1 by 0.13 L after 3 days of therapy (95% CI, 0.04 to 0.21). Meanwhile, the risk of hyperglycaemia significantly increased (relative risk, 5.88; 95% CI, 2.40 to 14.41)"
Indication:
- Exacerbations in patients with moderate to severe COPD.
- Should be avoided in stable COPD patients.
References:
Ipravent with Budecort:
Mechanism of action:
Decreases in inflammatory cytokines, C-reactive protein, and inflammatory cells have been observed with corticosteroid use, suggesting a possible mechanism for a therapeutic benefit of steroids.
Efficacy over placebo:
Budesonide and ipratropium bromide have shown improved lung function and measures of dyspnea when compared with placebo or either individual component
"Combined treatment improved QOL and decreased the rate of exacerbation, particularly in patients with an FEV1 of less than 50% predicted (71). Patients with severe COPD may show particular benefit to combined ICS and LABAs as when compared with LABAs alone because patients with an FEV1 of less than 50% predicted had a 35% reduction in moderate and severe COPD exacerbations over a 44-week study period"
Indications:
- Acute exacerbation of moderate to severe COPD.
- Stable COPD
References :
Inj HAI:
Insulin therapy is given to this patient because she is a known diabetic and insulin plays a role in sending the glucose in to the cells thereby maintaining the glucose levels in the body.
Inj Thiamine:
Mechanism of action:
Thiamine is a cofactor for pyruvate dehydrogenase, an essential enzyme for aerobic metabolism. In thiamine deficiency, pyruvate cannot enter the Krebs cycle, and anaerobic metabolism takes over. Decreased ATP production, vasodilatory shock, and lactic acidosis ensue. Thiamine administration rapidly reverses these effects in patients with thiamine deficiency.
Efficacy over placebo:
The administration of a single dose of thiamine was associated with a trend toward increase in o2 in critically ill patients. There was a significant increase in o2 in those patients with preserved or elevated CI. Further study is needed to better characterize the role of thiamine in oxygen extraction.
Twenty patients were enrolled and 3 were excluded because of incomplete o2 data, leaving 17 patients for analysis. There was a trend toward increase in o2 after thiamine administration (16.3 ml/min, SE 8.5; P = 0.052). After preplanned adjustment for changes in CI in case of a delivery-dependent state in some patients (with exclusion of one additional patient because of missing CI data), this became statistically significant (16.9 ml/min, SE 8.6; P = 0.047). In patients with average CI greater than our cohort’s mean value of 3 L/min/m2, o2 increased by 70.9 ml/min (±16; P < 0.0001) after thiamine. Thiamine had no effect in patients with reduced CI (< 2.4 L/min/m2). There was no association between initial thiamine level and change in o2 after thiamine administration.
Indications:
-Critically ill patients
-Patient’s with low oxygen levels in the body
ANSWER:
The cause for her exacerbation can be due to:
- Continuous exposure to various organisms such bacteria, fungi, and viruses during her working period in the paddy fields and also also exposure to the environmental pollutants.
- Daily exposure to the smoke released by the indoor chulka which is used in a room with improper ventilation
- The patient might have been allergic to the organisms present in tha paddy husk which is removed during the months of January which have have exacerbated her shortness of breath everytime she goes to the fields.
4. Could the ATT have affected her symptoms? If so how?
ANSWER:
The patient immediately developed generalised weakness on starting the ATT which might have been due to the side effects of the various drugs that are taken rifampicin, isoniazid, and pyrazinamide.
The patient also developed pedal edema and puffiness if the face after starting the anti tubercular therapy which might have been due to various commonly developing side effects of the drugs such as hepatitis, renal failure etc.
5. What could be the causes for her electrolyte imbalance?
ANSWER:
The people suffering from COPD suffer from various types of electrolyte abnormalities such as
hyponatremia, hypokalemia, hyperbilirubinemia, elevated transaminases, elevated blood urea, and elevated serum creatinine which might be due to various causes either due to disease process or may be due to the treatment given.
The patient suffering from COPD grave increased levels of CO2 in their body leading to various compensatory mechanisms one of which is decreasing the renal blood flow leading to retention of sodium and water hence there is sodium retention in the body which also affects other electrolytes such as potassium and chloride leading to their abnormal levels
The patient is also on Anti tubercular therapy which may further aggravate the electrolyte abnormalities due to the side effects of the drugs leading renal failure , sodium buildup etc.
NEUROLOGY
CASE AND DISCUSSION :
A) A 40 year old male presented to hospital from Yadagirigutta with chief complaints of irrelevant talking and decreased food intake since 9 days.
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localisation for the problem and what is the primary aetiology of the patient's problem?
Answer:
a) Symptomatology in the patient in terms of an event timeline :
1 year back :
History of 2-3 episodes of seizures 1 year back
4 months back :
Cessation of alcohol for 24 hrs
↓
1 episode of seizure (most probably a GTCS)
↓
Associated with restlessness, sweating, tremors
10 days back :
Generalized body pains
9 days back :
Stopped consuming alcohol since this day due to generalised body pains on the previous day
↓
-Started talking to himself and laughing to himself (sudden onset)
-Conscious , but oriented to time, place and person only from time to time
-Unable to lift himself from bed and move around
-Decrease in food intake
-Short term memory loss and unable to identify family members from time to time
↓
Taken to a local RMP, given I.V fluids and reffered to a higher care facility
↓
Admitted to tertiary care hospital on 15th may
b) Anatomical localisation of the problem :
- Acute symmetrical lesions in thalamus , mamillary bodies , tectal plates , periaqueductal area , floor of 4rth ventricle (includes occulomotor and vestibular nuclei and cerebellar vermis)
- lesions in the form of vascular congestion, microglial perforation and petechial hemorrhages.
c) Primary etiology for the patient's condition:
- Primary etiology for the patient's conditions is chronic alcoholism and dependance
- This lead to a chronic thiamine deficiency leading to wernicke's encephalopathy
- Alcohol dependance lead to symptoms of swearting , restlessness, and seizures as withdrawal symptoms on stoppage of alcohol.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer:
Inj. 1amp Thiamine in 100ml NS,TID
Mechanism of action:
Thiamine is useful in preventing Wernicke encephalopathy, an acute disorder due to thiamine deficiency manifested by confusion, ataxia, and ophthalmoplegia, as well as the chronic Korsakoff syndrome, which is manifested by memory impairment and amnesia
Indication of thiamine:
Thiamine has been recommended to be used to wernicke's to combat the deficiency of thiamine in the patient presenting with wernicke's
Efficacy over placebo:
'Patients with suspected WE were treated with ≥500 mg intravenous thiamine for a median of 3 days with 73% of patients (eight out of eleven) displaying symptom resolution or improvement after treatment.'
Inj. Lorazepam
Mechanism of action:
Lorazepam binds to benzodiazepine receptors on the postsynaptic GABA-A ligand-gated chloride channel neuron at several sites within the central nervous system (CNS). It enhances the inhibitory effects of GABA, which increases the conductance of chloride ions into the cell. Thereby helping in controlling seizures which are due to increased electric impulses of brain
Indications of lorazepam:
Lorazepam is used in alcohol withdrawal in cases of
• patients with severe liver dysfunction
• patients who are at high risk of experiencing serious medical consequences following sedation
• people with severe lung disease
• elderly patients
References :
T.Pregabalin
Mechanism of action :
Pregabalin works in different ways: in epilepsy it stops seizures by reducing the abnormal electrical activity in the brain. with nerve pain it blocks pain by interfering with pain messages travelling through the brain and down the spine.
Efficacy over placebo:
'Alcohol withdrawal symptoms and craving for alcohol resulted significantly reduced (p < 0.001) over time after pregabalin treatment. Pregabalin also resulted in a favourable improvement in psychiatric symptoms and quality of life (p < 0.001).'
Indications:
•Associated psychiatric symptoms in patients with alcohol withdrawal symptoms
•Seizure prone patients of alcohol withdrawal
•Anxiety, hostility and psychoticism in patients of alcohol withdrawal
Inj. HAI s.c - premeal and GRBS
Mechanism of action:
HAI is a short-acting insulin. It works by helping blood sugar (glucose) get into cells so your body can use it for energy. GRBS stands for General Random Blood Sugar. Due to the deficiency of Vit.B1 patients of wernicke's encephalopathy cannot utilise the glucose in their body and hence require short term insulin to be administered in the presentation to hospital.
Efficacy over placebo:
•Insulin helps in transferring the glucose into the cell for the utilisation in the cells.
•Insulin helps in treating the patients presenting with diabetic coma
• However ,Insulin and glucose should not be administered before the administration of thiamine in a chronic alcoholic as they may precipitate wernicke's encephalopathy.
Indications:
•chronic alcoholics presenting with diabetic ketoacidosis
•chronic alcoholics presenting in the comatosed state
Lactulose 30ml/PO/BD
Mechanism of action :
Lactulose is used in preventing and treating clinical portal-systemic encephalopathy. Its chief mechanism of action is by decreasing the intestinal production and absorption of ammonia. It has also gained popularity as a potential therapeutic agent for the management of subacute clinical encephalopathy.
Efficacy over placebo:
Compared with placebo or no intervention, lactulose significantly reduced the risk of no improvement in neuropsychological tests (RR: 0.52, 95% CI: 0.44–0.62, P<0.00001), the time required for the completion of the number connection test-A (WMD: −26.95, 95% CI: −37.81 to −16.10, P<0.00001), and the mean number of abnormal neuropsychological tests (WMD: −1.76, 95% CI: −1.96 to −1.56, P<0.00001). Furthermore, the meta-analysis also showed that lactulose prevented the progression to overt hepatic encephalopathy (RR: 0.17, 95% CI: 0.06–0.52, P=0.002), reduced blood ammonia levels (WMD: −9.89 µmol/l, 95% CI: −11.01 to −8.77 µmol/l, P<0.00001), and improve health-related quality of life (WMD: −6.05, 95% CI: −6.30 to −5.20, P<0.00001). However, no significant difference was observed in the mortality of patients with MHE (RR: 0.75, 95% CI: 0.21–2.72, P=0.66), and lactulose significantly increased the incidence of diarrhea (RR: 4.38, 95% CI: 1.35–14.25, P=0.01).
Indications:
•Acute onset of severe encephalopathy symptoms
•Minimal hepatic encephalopathy
•chronic alcoholism
Inj. 2 amp of KCl
Mechanism of action:
Potassium ions participate in a number of essential physiological processes, including the maintenance of intracellular tonicity; the transmission of nerve impulses; the contraction of cardiac, skeletal, and smooth muscle; and the maintenance of normal renal function.
Efficacy over placebo:
In a patient with hypertension due to hypokalemia given with KCl therapy caused an average rise in the serum potassium concentration of 0.56 mmol per liter, the mean blood pressure fell by an average of 5.5 mm Hg (P = 0.004), with at least a 4 mm Hg fall observed in 9 of the 16 patients. The fall in blood pressure correlated with a fall in plasma renin activity (r = 0.568, P = 0.043) but not with changes in plasma aldosterone levels or other variables.
Indications:
•hypokalemia
•uremia
•metabolic acidosis
•insulin therapy given
•intermittent iv infusions
3)Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
The patient experienced withdrawal symptoms first time he stopped consuming alcohol, but they were not as severe as this time. This time when he stopped consuming alcohol he experienced severe withdrawal symptoms which had even neurological side effects such as short term memory loss, psychosis, and unable to lift his body and move around.
This is due to potentiation of the withdrawal symptoms when the patient relapses and takes alcohol again after absconding from alcohol. The next time he withdraws alcohol the symptoms will be much more severe.
This is the reason why the patient did not have neurological symptoms last time when he stopped alcohol.
4) What is the reason for giving thiamine in this patient?
Answer:
Chronic alcoholics have high incidence of vitamin B1(thiamine) deficiency and this is the main reason for the wernicke's encephalopathy in this patient cjasing a lot of neurological symptoms in the patient. Thiamine is thus given as a prophylactic and treatment therapy of wernicke's encephalopathy.
5) What is the probable reason for kidney injury in this patient?
Answer:
The main reason for kidney injury in this patient is due to his chronic alcohol consumption.
The kidneys filter harmful substances from your blood. One of these substances is alcohol. Alcohol can cause changes in the function of the kidneys and make them less able to filter your blood. In addition to filtering blood, kidneys do many other important jobs. One of these jobs is keeping the right amount of water in your body. Alcohol affects the ability of your kidneys to do this. When alcohol dehydrates (dries out) the body, the drying effect can affect the normal function of cells and organs, including the kidneys.
Too much alcohol can also affect the blood pressure. People who drink too much are more likely to have high blood pressure. And medications for high blood pressure can be affected by alcohol. High blood pressure is a common cause of kidney disease. More than two drinks a day can increase chance of having high blood pressure.
Chronic drinking can also cause liver disease. This adds to the kidney's job. The rate of blood flow to your kidneys is usually kept at a certain level, so that your kidneys can filter your blood well. Liver disease impairs this important balancing act. In fact, most patients in the United States who have both liver disease and associated kidney dysfunction are alcohol dependent.
References :
6) What is the probable cause for the normocytic anemia?
Answer:
Most often, however, normocytic anemia is acquired — meaning it develops later as a result of another cause, such as a disease.
This is known as anemia of chronic disease (ACD) or anemia of inflammation, because the diseases that can lead to normocytic anemia cause inflammation in certain parts of the body or throughout the body.
The patient has chronic alcoholism which lead to a chronic kidney disease which might have been the cause for normocytic anemia.
The patient is also malnourished due to his chronic alcoholism and hence may also be the reason for normocytic anemia
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why
Answer:
Chronic alcoholism is a main cause of peripheral neuropathy which may be a main cause for the development of repeated ulcers on the foot.
Alcoholic neuropathy is one of the most common and least recognizable consequences of heavy alcohol use. People with a long history of alcohol misuse might experience pain, tingling, weakness, numbness, or loss of balance as a result of alcoholic neuropathy.
This neuropathy might be the main cause for the formation in foot ulcer in the patient.
B) A 52 year old male came to the hospital 2 days back presenting with slurring of speech and deviation of mouth that lasted for 1 day and resolved on the same day.
Patient details :
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer:
a) Symptomatology in the patient in terms of an event timeline:
7 days back:
- 1 episode of giddiness which later subsided on taking rest
- 1 episode of vomitings
↓
3days back:
- Consumed a little bit of alcohol
- Got another episode of dizziness which was sudden in onset, continuous and gradually progressive
-It was increasing on standing up and walking
- Associated with bilateral hearing loss, aural fullness and presence of tinnitus
- This was associated with Bilateral Hearing loss, aural fullness and presence of tinnitus.
Patient has H/o postural instability- he is unable to walk without presence of supports, swaying is present and he has tendency to fall while walking
b) Anatomical localisation :
Cerebellar infarct revealed on the CT Scan images.
c) Primary etiology in causing the disease :
Patient being a chronic hypertensive and a chronic alcoholic might have been the primary etiology in causation of the disease.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Answer :
Tab Veratin 8 mg PO TID
Mechanism of action :
The active ingredient of Betahistine is Betahistine hydrochloride or Betahistinedemesytate. Betahistine is one of the few drugs known which is said to improve the microcirculation of the inner ear. It works as a histamine analogue through 2 modes of action(1) agonist of H1 receptors and (2) antagonist of H3 receptors. It has a weak effect on H1 receptors but strong effect on H3 receptors.Betahistine is thought to work by increasing the blood flow around the inner ear. This reduces the amount of fluid in the inner ear and prevents symptoms from developing.
Efficacy over placebo :
Several clinical trials have demonstrated that betahistine is effective in reducing the frequency and severity of vertigo, and improving vertigo-associated symptoms, including nausea and vomiting
Cochrane Review of randomised controlled trials of betahistine versus placebo in patients with symptoms of vertigo suggested that betahistine may have a positive effect in terms of reduction in vertigo symptoms
Indications :
•Ménière's syndrome
•vertigo
•tinnitus
•hearing loss and
•nausea
Inj. Zofer 4mg IV/TID
Mechanism of action:
Zofer Tablet works by inhibiting the action of a chemical substance named serotonin, which is responsible for inducing nausea and vomiting. Ondansetron binds to a receptor known as 5-HT₃, thus inhibits the binding of serotonin to it and prevents vomiting and nausea
Indications :
•Nausea and vomiting due to certain medical conditions like stomach upset
•Nausea and vomiting caused due to any surgery, cancer drug therapy or radiotherapy.
Efficacy over placebo :
For every 100 patients receiving an adequate dose of ondansetron 20 patients will not vomit who would have vomited had they received placebo. The antinausea effect is less pronounced. Of these 100, three will have elevated liver enzymes and three will have a headache who would not have had these adverse effects without the drug
Tab. Ecosprin 75mg PO/OD
Mechanism of action :
Ecosprin provides the antiplatelet action by irreversibly inhibiting the formation of thromboxane A2, via acetylation of platelet cyclooxygenase.
Indications:
•For prevention of blood clot formation in individuals with a high risk of clotting in blood vessels.
•For prevention of heart attack.
•For prevention of cerebellar infarct due to a clot formation.
•For treatment of an Cardiovascular infarct/Stroke
Efficacy over placebo:
Aspirin started early in hospital produces a small but definite net benefit, with about 9 (SD 3) fewer deaths or non-fatal strokes per 1000 in the first few weeks (2p=0·001), and with 13 (5) fewer dead or dependent per 1000 after some weeks or months of followup (2p<0·01).
Tab. Atorvastatin 40mg PO/HS
Mechanism of action:
Atorvastatin competitively inhibits 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase. By preventing the conversion of HMG-CoA to mevalonate, statin medications decrease cholesterol production in the liver
Indications : Clinicians may choose to offer a low- to moderate-dose statin to certain adults without a history of CVD when all of the following criteria are met: 1) they are aged 40 to 75 years; 2) they have 1 or more CVD risk factors (i.e., dyslipidemia, diabetes, hypertension, or smoking); and 3) they have a calculated 10-year risk of a cardiovascular event of 7.5% to 10%
Efficacy over placebo :
Compared with placebo, standard-dose statin treatment resulted in a significant relative risk (RR) reduction of 15% in the occurrence of any major cardiovascular or cerebrovascular event (RR 0.85, 95% CI 0.79–0.91). Compared with standard-dose statin treatment, intensive-dose statin treatment resulted in an additional 9% relative risk reduction (RR 0.91, 95% CI 0.84–0.98).
Tab. Clopidogrel 75mg PO/OD
Mechanism of action:
The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation.
Indications :
FDA-approved indications for clopidogrel include:
-Use during a percutaneous coronary intervention (PCI) for acute coronary syndrome (ACS) and stable ischemic heart disease.
-Primary prevention of thromboembolism atrial fibrillation
-Symptomatic carotid artery stenosis
-Secondary prevention post-coronary artery bypass grafting
-Peripheral artery percutaneous angioplasty in •peripheral artery bypass grafting
Efficacy over placebo :
The CREDO trial, PCI-CURE subset analysis, and ISAR studies support the benefit of early treatment with clopidogrel before PCI. The combined analysis of these studies clearly indicates that adequate inhibition of platelet function with clopidogrel and aspirin alone can be achieved in troponin-negative patients without a need for a Gp IIb/IIIa inhibitor on board.
References :
Inj. Thiamine 1 amp in 100ml NS PO/BD
Mechanism of action :
Thiamine is useful in chronic alcoholics in preventing Wernicke encephalopathy in , an acute disorder due to thiamine deficiency manifested by confusion, ataxia, and ophthalmoplegia, as well as the chronic Korsakoff syndrome, which is manifested by memory impairment and amnesia.
Indications :
• In conditions of thiamine deficiency commonly noticed in chronic alcoholics with presenting symptoms of beri beri and wernicke's encephalopathy
• In malabsorption disorder caused due to chronic alcoholism
• In patients with chronic alcoholism and associated psychiatric symptoms.
Efficacy over placebo :
Thiamine is commonly used for the treatment of wernicke's encephalopathy and has also been recommended as the first drug to be administered in all the complications due to alcoholism in chronic alcoholics.
3) Did the patients history of denovo HTN contribute to his current condition?
Answer :
Yes , the incidence of strokes increased in the presence of hypertension. Hence the hypertension in the patient might have contributed to the present condition
High blood pressure can also cause blood clots to form in the arteries leading to your brain, blocking blood flow and potentially causing a stroke.
The crude incidence of stroke was 289/100000 person-year in controlled hypertensive subjects and 705/100000 person-year in treated hypertensive subjects with BP 140/90 mm Hg. It was estimated that 45% of all strokes among subjects with treatment for hypertension might be attributed to uncontrolled BP.
HTN is a major risk factor associated with 67%(70.104) of patients with AIS. Multivariate analysis suggests higher odds of 4.088(95%Cl, 0.721–23.179) and 2.437(95%Cl, 0.721–23.179) for 12 and 18 months outcome in patients with AIS and HTN, respectively.
References :
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
Answer :
Heavy drinking should be considered as one of the risk factors for hemorrhagic stroke. In contrast to the protective effect of mild-to-moderate alcohol use against ischemic strokes, moderate drinking might result in an increased risk of hemorrhagic strokes
Most case-control and cohort studies either reported only on total strokes or on a combined group of hemorrhagic strokes including intracerebral as well as subarachnoid hemorrhages. There was a consensus among reports that heavy alcohol consumption was associated with a higher risk of hemorrhagic strokes. Controversy remains regarding the effect of mild-to-moderate alcohol consumption: while some studies reported a protective effect, others found a dose-dependent linear relationship between the amount of alcohol consumed and the risk of hemorrhagic stroke.
C) A 45 years old female ,house wife by occupation came to opd with chief complaints of palpitations,chest heaviness,pedal edema,chest pain,radiating pain along her left upper limb
QUESTIONS :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer :
8 months back:
-Apparently normal
-Then she developed bilateral pedal edema which are gradually progressing and was present on both sitting and standing positions
-Relieved on taking medication
↓
6 days back:
-Pain radiating along left upper limb which was dragging in nature
-Aggravated during palpitations and relieved on taking medication for palpitations
-Chest pain associated with chest heaviness
↓
5 days back:
-Palpitations which were sudden in onset, more during night time
-Aggravated on lifting weights, speak continuously
-Relieved by drinking more water and taking medication
-Dyspnoea during palpitations (NYHA-CLASS-3)
-No history of fever/vomiting/diarrhoea/muscle pain
b) Anatomical localisation :
The main problem which is leading to all the symptoms is cervical spondylosis which can lead to compression of all the nerve roots and/or the spinal cord which may have caused most of the symptoms such as pain and tingling along the left upper limb etc
The patient also has hypokalemia which has caused paralysis due to weakness in various muscles leading to their flaccid paralysis hence causing periodic intermittent paralysis.
c) Primary etiology in the problem :
-The primary etiology is the old age of the patient which has lead to cervical spondylosis in the patient .
-There may also be genetic causes which might have predisposed her to lead to this condition.
-Hypokalemic periodic paralysis may also have been inherited in a genetic manner.
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
Hypokalemic periodic paralysis is usually inherited in a genetic manner in autosomal dominant fashion and hence recurs very commonly in the patient leading to repeated episodes of paralysis in the patient,
Risk factors for hypokalemia:
-Due to medications such as diuretics, enema, laxatives etc
-Due to inadequate intake such as in starvation, dementia, anorexia
-Due to trans cellular shift in conditions such as alkalosis, thyrotoxicosis, delirium, tremors
-Due to renal causes such osmotic diuretics, mineralocorticoid excess, renal tubular acidosis
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
Answer :
a)Ecg findings :
•3-3.5 meq/L : Flatenning of T wave , Prominent U wave and Prominent QT interval
•2.5-3 meq/L : Sagging or depression of ST segment
• <2.5 meq/L : QRS widening , increased risk of arrythmia , PR prolongation.
b) Symptoms of hypokalemia :
•Weakness
•Fatigue
•Muscle cramps or twitching
•Constipation
•Arrhythmia
•Worsening diabetes control or polyuria.
•Palpitations.
•Psychological symptoms (eg, psychosis, delirium, hallucinations, depression)
D) A 55year old male patient came to opd with c/o altered sensorium and involuntary movements from 11pm and recurrent episodes of seizures since 5yrs.
QUESTIONS:
1) Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
Answer :
Relationship Between Seizure and Stroke:
Strokes can damage the brain in many ways, and these negative effects take different forms depending on the person and their stroke. But in general, strokes can influence emotions, mobility, verbal communication, behavior, and memory. One problem caused by stroke that’s harder to notice is the increased risk of seizures.
Seizures are actually more common after stroke. Statistics show that seizures afflict 22 percent of people who suffer from strokes. They are important to watch out for as they indicate malfunctions in brain activity and cause an altered state of awareness for a stretch of time.
There are several causes for early onset seizures after ischaemic strokes. An increase in intracellular Ca2+ and Na+ with a resultant lower threshold for depolarisation, glutamate excitotoxicity, hypoxia, metabolic dysfunction, global hypoperfusion, and hyperperfusion injury (particularly after carotid end arterectomy) have all been postulated as putative neurofunctional aetiologies. Seizures after haemorrhagic strokes are thought to be attributable to irritation caused by products of blood metabolism. The exact pathophysiology is unclear, but an associated ischaemic area secondary to haemorrhage is thought to play a part. Late onset seizures are associated with the persistent changes in neuronal excitability and gliotic scarring is most probably the underlying cause. Haemosiderin deposits are thought to cause irritability after a haemorrhagic stroke.14 In childhood, post‐stroke seizures can occur as part of perinatal birth trauma.
If you’ve suffered from hemorrhagic (bleeding) strokes, you’re much more likely to experience seizures post stroke than those who’ve suffered from an ischemic stroke. You’re also more likely to experience seizures if a stroke takes place in the cerebral cortex, the outer layer of tissue in the brain.
2) In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Answer:
The patient in the previous episodes of seizures had a simple partial seizure but in the recent episode she had a complex partial seizure which resulted in a tonic clinic seizure which resulted in a seizure with loss of consciousness.
Partial seizures can be simple or complex. Unlike complex partial seizures simple seizures usually have seizure with unilateral paralysis and there is no alteration of consciousness. Secondary generalisation occurs when partial seizures spread to both sides of the brain which results in tonic clonic seizures and lord of consciousness.
This is phenomenon is called as ‘Complex partial seizure secondarily generalised’.
E) A 48-year-old gentleman hailing from a small town in Telangana presented to the casualty ward on 25th April 2021 at 7:40am with the chief complaints of unresponsiveness for 7 hours and 3 intermittent episodes of seizures in the past 3 hours
Patient details :
QUESTIONS :
1) What could have been the reason for this patient to develop ataxia in the past 1 year?
Answer :
Alcohol induced cerebellar degeneration is the commonest type of acquired toxic ataxia. The onset of the cerebellar symptoms usually occurs at middle age, with a significant history of chronic alcohol abuse. Permanent cerebellar deficits are observed among alcoholics, and they persist even with alcoholic abstinence.
A total of 78 chronic alcoholics were examined neurologically as well as by electroneurography, myography and posturography. Clinical signs of peripheral neuropathy were detected in 45% of these patients, with electromyographic and neurographic abnormality in 67% and 55% respectively. Clinical signs of cerebellar ataxia were found in 33% of our patients, whereas posturographic measurements of increased sway were recorded in 69%. The posturographic characteristics of cerebellar anterior lobe atrophy were observed in two-thirds of the latter patients. The severity of cerebellar-ataxia did not correlate with the degree of neuropathy. This lack of correlation is interpreted as an indication of different pathogenetic mechanisms acting on peripheral nerves and cerebellum.
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
Answer :
The most probable reason for the Intracranial bleed in the patient might be chronic alcoholism. Chronic alcoholism has been equated to increased risk and chances of causing intracranial bleeding. It's not clear exactly how alcohol affects stroke risk, but some theories center on the fact that alcohol thins your blood. This could increase your risk of hemorrhagic stroke, in which a blood vessel breaks inside the brain.
Heavy alcohol consumption demonstrated a strong association with increased nonlobar ICH risk (OR 2.04, p = 0.0003). Heavy alcohol consumption was associated with significant increase in nonlobar ICH risk in black (OR 2.34, p = 0.0140) and Hispanic participants (OR 12.32, p < 0.0001).
F) A 30 year old male patient with weakness of right upperlimb and lowerlimb, deviation of mouth towards left
QUESTIONS :
1) Does the patient's history of road traffic accident have any role in his present condition?
Answer :
The patient's MRI indicated the presence of 'Altered signal intensity areas involving left caudate nucleus, left frontal and temporal regions, that is hyperintense on T2/FLAIR with evidence of diffuse restrictions and loss of grey white matter differentiation
These findings are indicative of Acute infarct in the Middle Cerebral Artery territory without any evidence of hemorrhages.
These infarcts might be consistent with the finding in the history of the patient which has a road traffic accident mentioned as Post-traumatic cerebral infarction (PTCI) is one of the most severe secondary insults after traumatic brain injury (TBI), and is known to be associated with poor outcome and high mortality rate
Important findings :
Of the 986 patients with TBI in this study, cerebral infarction was observed in 21 patients (2.1%) within 3 months after trauma. In one retrospective cohort study, the prevalence of cerebral infarction was 1.9%.12) Other studies revealed that prevalence of PTCI was up to 10.4%.19,21,22) These studies included only moderate or severe brain trauma patients. However, patients with TBI of all grades of severity were enrolled in this investigation. Therefore, our result showed low incidence of PTCI compared to other studies. When excluding patient with GCS score of 12 to 15, incidence of PTCI was 6.9%.
2)What are warning signs of CVA
Answer:
The five warning signs of CVA/Stroke are:
•Sudden onset of weakness or numbness on one side of the body
•Sudden speech difficulty or confusion
•Sudden difficulty seeing in one or both eyes
•Sudden onset of dizziness, trouble walking or loss of balance
•Sudden, severe headache with no known cause
3)What is the drug rationale in CVA?
Answer:
The Role of Medications in General Supportive Care:
•Oxygenation
Maintaining adequate tissue oxygenation is important during periods of acute cerebral ischemia in order to prevent hypoxia and potential worsening of the neurologic injury.
•Antihypertensives
In the setting of AIS, many patients will have elevated blood pressure for the first 24–48 hours. Although severe hypertension is a contraindication for thrombolytic therapy, there are no data to define the levels of arterial hypertension that mandate emergent management.
•Insulin
Hypoglycemia can cause focal neurologic signs that mimic stroke and can itself lead to brain injury. Additionally, several clinical studies have associated hyperglycemia with poor outcomes.[7,8] Therefore, prompt measurement and normalization of serum glucose concentration is important.
•Antipyretics
Increased body temperature in the setting of acute ischemic stroke has been associated with poor neurologic outcome, possibly due to increased metabolic demands, enhanced release of neurotransmitters, and increased free radical production.
Rationale of drugs in the treatment of Acute Ischemic Stroke:
•Thrombolysis
Intravenous administration of alteplase is the only US Food and Drug Administration (FDA)-approved medical therapy for treatment of patients with acute ischemic stroke. Its use is associated with improved outcomes for a broad group of patients. Recent trials have shown the therapeutic window may be extended out to 4.5 hours in selected patients.
•Device Therapies
Mechanical thrombectomy delivered endovascularly is another option for clot removal, either as an adjunct to thrombolysis or for patients who are ineligible for IV alteplase.
•AnticoagulantsData suggest that urgent anticoagulation in unselected acute ischemic stroke patients leads to symptomatic intracranial hemorrhage that outweighs any potential benefit.Heparin UFH has its anticoagulant effects by inactivating thrombin and activated factor X.
•Antiplatelet Agents
Aspirin irreversibly inhibits cyclooxygenase, which prevents the conversion of arachidonic acid to thromboxane A2 (TXA2). Thromboxane A2 is a vasoconstrictor and stimulator of platelet aggregration.
Clopidogrel irreversibly blocks ADP receptors on platelets and thus prevents the cascade resulting in activation of GP IIb/IIIa receptor.
The CAPRIE (Clopidogrel versus Aspirin in Patients at Risk of Ischaemic Events) trial tested clopidogrel 75 mg daily versus aspirin 325 mg daily in the prevention of cardiovascular and cerebrovascular events.
•Mannitol is an osmotic diuretic, typically used at 0.25–0.5 g/kg IV administered over 15 minutes. It lowers intracranial pressure, and can be given every 6 hours.[76] The usual maximal dose is 2 g/kg. Its effect in patients with ischemic brain swelling is still unknown, but it is often used as a temporizing measure before patients undergo decompressive craniectomy.
4)Does alcohol has any role in his attack?
Answer :
Liver damage due to too much alcohol can stop the liver from making substances that help your blood to clot. This can increase your risk of having a stroke caused by bleeding in your brain. It is also debated that alcohol may exhinit a protective effect on ischemic strokes.
But in the patient history it has been described that the patient is an occasional alcohol consumer and also he had not consumed any alcohol prior to the attack indicates that alcohol might not have any role to play in the causation of this disease.
5)Does his lipid profile has any role for his attack??
Answer :
The patient has lower levels of HDL in his body while the other parameters of lipid profile are normal.
Studies have demonstrated a trend toward a higher risk of stroke with lower HDL-C and support HDL-C as an important modifiable stroke risk factor. In patients with recent stroke or transient ischemic attack and no coronary heart disease, only lower baseline HDL-C predicted the risk of recurrent stroke
Higher HDL cholesterol and a higher concentration of large particles are associated with lower risk of stroke
G)50-year-old male patient presented to hospital with complaints of weakness of all four limbs since 8 PM yesterday.
QUESTIONS :
1)What is myelopathy hand ?
Answer :
A characteristic dysfunction of the hand has been observed in various cervical spinal disorders when there is involvement of the spinal cord. There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement. The characteristic nature of the signs permit the distinction between myelopathy and changes due to nerve root or peripheral nerve disorder.
The main clinical features are localized wasting and weakness of the extrinsic and intrinsic hand muscles, but not accompanied by either sensory loss or spastic quadriparesis. For an accurate diagnosis, attention should be paid to the narrow anteroposterior (AP) canal diameter of the cervical spine (less than 13mm), multisegmental spondylosis in C5-6 and C6-7 disc levels and a reduced transectional area of the spinal cord at the C7, C8, or T1 spinal cord segments. To date the authors have seen 15 patients with this hand; seven underwent either spondylectomy or laminoplasty. In six patients who were satisfied with surgical results, recovery from muscle wasting and weakness was seen.
2)What is finger escape ?
Answer:
Wartenberg's sign is a neurological sign consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi.
It may be due to : Ulnar nerve neuropathy ,Cervical myelopathy, Upper motor neuron disorders of the cerebral cortex (such as mild hemiplegic stroke or hemiplegic migraine where the same clinical finding has been called the "digiti quinti sign")
This commonly results from weakness of some of the ulnar nerve innervated intrinsic hand muscles -in particular the palmar interosseous muscle to the little finger- caused by damage to their nerve supply (denervation). There may be different causes for this denervation and muscle imbalance including:
3)What is Hoffman's sign?
Answer:
The Hoffman sign is an involuntary flexion movement of the thumb and or index finger when the examiner flicks the fingernail of the middle finger down. The reflexive pathway causes the thumb to flex and adduct quickly. A positive Hoffman sign indicates an upper motor neuron lesion and corticospinal pathway dysfunction likely due to cervical cord compression. However, up to 3% of the population has been found to have a positive Hoffman without cord compression or upper motor neuron disease.
H) A 17 year old female student by occupation presented to causality with complaints of involuntary movements of both upper and lower limbs
QUESTIONS :
1) What can be the cause of her condition ?
Answer :
As the MRI indicates the patient has Acute cortical vein thrombosis with hemorrhagic venous infarction involving Right posterior temporal lobe with midline shift to left by 4mm.
The patient is also suffering from severe iron deficiency anemia. Iron deficiency anemia can increase the number of platelets in blood, which is linked with a hypercoagulable state. Erythropoietin which stimulates megakaryocytes is also increased during the iron deficiency.
Iron deficiency in itself can lead to a hypercoagulable state. It has been found that microcytosis decreases the cell deformability and increase the viscosity, causing abnormal flow patterns.Under conditions of stress or infections, the metabolic demand at the tissue level rises which can create anemic hypoxia and can predispose to venous thrombosis.
2)What are the risk factors for cortical vein thrombosis?
Answer:
Risk factors for children and infants include:
•Problems with the way their blood forms clots
•Sickle cell anemia
•Chronic hemolytic anemia
•Beta-thalassemia major
•Heart disease — either congenital (you're born with it) or acquired (you develop it)
•Iron deficiency
•Certain infections
•Dehydration
•Head injury
•For newborns, a mother who had certain infections or a history of infertility
Risk factors for adults include:
•Pregnancy and the first few weeks after delivery
•Problems with blood clotting; for example, antiphospholipid syndrome, protein C and S deficiency, antithrombin III deficiency, lupus anticoagulant, or factor V Leiden mutation
•Cancer
•Collagen vascular diseases like lupus, Wegener’s granulomatosis, and Behcet syndrome
•Obesity
•Low blood pressure in the brain (intracranial hypotension)
•Inflammatory bowel disease like Crohn’s disease or ulcerative colitis
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
Answer:
Levipil is an anti-epileptic drug used to treat epilepsy seizures (fits). It can be used alone or in combination with other medications. It works to avoid seizures as long as you keep taking it. Levipil 500 Tablet works by reducing irregular brain electrical activity
After the stat iv administration of levipil there was a seizure - free period due to the action of the antiepileptic and as soon as the dosage of the drug got worned out the patient started experiencing seizures again.
Then the doctors administered inj. phenobarbitone 20mg/kg-800 mg iv stat. This cause spontaneous resolution of the seizures due to the rapid action of iv phenobarbitone in the resolution of seizures by decreasing brain activity.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Answer :
Clexane 0.4ml sc BD is the drug given in suspicion of cortical venous sinus thrombosis.
Clexane is one of a group of medicines called low molecular weight heparins (LMWH). These medicines work by reducing blood clotting activity.
Heparin anticoagulation is the time-honoured treatment, and is advocated in all cases of CVT, irrespective of etiology or presence of haemorrhage
3) CARDIOLOGY:
CASE AND DISCUSSION :
A) A 78 yr old male patient, came to the OPD with chief complaints of shortness of breath, chest pain, pedal edema and facial puffiness.
QUESTIONS:
1. What is the difference between heart failure with preserved ejection fraction and with reduced ejection fraction?
ANSWER:
Heart failure with preserved ejection fraction (HFpEF):
This condition occurs when the lower left chamber (left ventricle) is not able to fill properly with blood during the diastolic (filling) phase. The amount of blood pumped out to the body is less than normal. It is also called diastolic heart failure.
Risk factors include elderly females suffering from hypertension , diabetes mellitus and other comorbidities. Obesity has proven to be an important risk factor
Concentric Left ventricular remodeling has been observed along with cardiomyocyte hypertrophy, collagen lysis and interstitial fibrosis noticed on a molecular level. There occurs an increase in the left ventricular volume
Heart failure with reduced ejection fraction:
This condition occurs when the muscle of the left ventricle is not pumping as well as normal. The ejection fraction is 40% or less. The amount of blood being pumped out of the heart is less than the body needs.
Risk factors for this condition include males wit dyslipidemia , smoking and myocardial necrosis and inflammation.
Eccentric Left ventricular remodelling has been noticed along with cardiomyocyte loss, replacement fibrosis and low Left ventricular decreased volume on a microscopic level
2.
Why haven't we done pericardiocentesis in this patient? ANSWER:
It is avoided in the patient because:
-Normally pericardiocentesis is performed in patients with cardiac tamponade and as this patient does not have any cardiac tamponade it is not necessary.
-The patient has pericardial effusion but it’s size is very small(present as a small pocket) and can be resolved easily.The effusion was noticed to be reducing size (From2.4-1.9cm)
Pericardiocentesis is performed in cases of:
-In haemodynamically unstable patients, an emergent procedure is mandatory because only the removal of fluid allows a normal ventricular filling and restores an adequate cardiac output.
-In case of pericardial effusion without haemodynamic compromise, pericardiocentesis is indicated for symptomatic moderate to large effusion non-responsive to medical therapy, or in case of a smaller effusion, when tuberculous, bacterial or neoplastic pericarditis is suspected, or in case of chronic (lasting more than three months), large pericardial effusion (>20 mm on echocardiography in diastole).
Reference:
3. What are the risk factors for development of heart failure in the patient?
ANSWER:
The risk factors of the patient to be prone to heart failure are:
-Old age which decreases the threshold of heart to work and pump blood
-The patient is a chronic alcoholic and a chronic smoker. Both these conditions are very much in favour of increasing the chances of heart failure in the patient.
-The patient also has various heart problems such as Diastolic filling impairment, valvular heart disease and also collapsing left ventricle
-The patient also has many comorbidities such as diabetes mellitus and hypertension since many years which increase the chances of heart failure.
4. What could be the cause for hypotension in this patient?
ANSWER:
The patient is on high antihypertensive therapy including furosemide which might have been the cause for hypotension in the patient. However hypotension might have also been caused due to viral myocarditis or due to complete myocardial infarction.
Usually cardiac tamponade is commonly known to cause hypotension in the patient but here it was ruled out by performing a 2D echo hence it is not a cause.
B) A 73 yr male patient presented to OPD with chief complaints of pedal edema, shortness of breath and decreased urine output.
QUESTIONS :
1. What are the possible causes for heart failure in this patient?
ANSWER:
-The patient suffers from chronic hypertension and diabetes which are potential risk factors for heart failure.
-In addition to this the patient also has chronic kidney failure which further promotes the chances of occurrence of heart failure.
-The patient is also obese and has anemia which increase the load on heart thereby increasing chances of heart failure.
All these conditions might have caused the occurrence of heart failure in a mixed impact fashion
2. What is the reason for anemia in this case?
ANSWER:
Anemia may have been caused due to:
-The patient suffers from chronic kidney failure(CKD) and hence is at a high risk of anemia due to decreased synthesis of erythropoietin from the kidney as erythropoietin plays a major role in stimulation of erythropoesis.
-The patient is a chronic alcoholic and has increased chances of megaloblastic anemia due to decreased intake of folate through the diet, and also weak antifolate action of ethanol
-The patient also has an improper diet intake and hence may also be prone for iron deficiency anemia due to decreased intake of iron in diet.
-Overall the anemia may also be due to chronic disease or chronic alcoholism.
3. What is the reason for blebs and non healing ulcer in the legs of this patient?
ANSWER:
Diabetes has been known to rarely cause blebs and blisters. They are commonly a self limiting condition and diagnosis is often made clinically by the appearance of painless, tense blisters, arising from the inflamed skin.
Non healing ulcer is commonly caused due to delayed wounding healing been in conditions such as:
-Diabetes mellitus wherein there is narrowing of blood vessels leading to decreased perfusion
-Heart failure due to lower perfusion and oxygenation in the extremities
-Anemia can also halt or slow the wound healing stages, which leaves patients more susceptible to other complications such as wound infection.
4. What sequence of stages of diabetes has been noted in this patient?
ANSWER: stages of diabetes type 2 noted in the patient are:
Stage 1: insulin resistance
↓
Stage 2: prediabetes
↓
Stage 3: diabetes type
↓
Stage 4: microvascular complications ( retinopathy, nephropathy, neuropathy)
C) A 52yr old male came to the OPD with the chief complaints of decreased urine output and shortness of breath at rest and facial puffiness.
QUESTIONS:
1. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANSWER:
a) Symptomatology in this patient:
3 years ago:
-Facial puffiness
-Aggravation of pain at surgical site of a surgery done for inguinal hernia done 10 years back.
↓
1year ago:
-Shortness of breath( grade 2 , diagnosed to be hypertensive)
↓
since 2days
-Shortness of breath( started as grade 2 and progressed to grade 4)
-Decreased urine output
-Anuric since morning
.
b)The anatomical location of the disease/problem is:
Ther is presence of thrombi in regions of left atrial appendages and left atrium of the heart
There is also presence of dilation of all heart chambers and IVC.
c) Primary etiology: The causes of atrial fibrillation with thrombus formation in the patient are:
-Pulmonary artery hypertension
-Congestive cardiac failure
2. What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Dobutamine Inj:
Mechanism of action:
Dobutamine is a synthetic catecholamine that acts on alpha-1, beta-1 and beta-2 adrenergic receptors. In the heart, the stimulation of these receptors produces a relatively strong, additive inotropic effect and a relatively weak chronotropic effect
Efficacy over placebo :
Fourteen studies, with 673 participants, met the inclusion criteria and were included; 13 studies reported mortality. There was minimal heterogeneity (I 2 = 4.5%). The estimate of the odds ratio for mortality for patients with severe heart failure treated with dobutamine compared with standard care or placebo was 1.47 (95% confidence interval 0.98–2.21, p = 0.06).
Indications:
-Cardiogenic shock with a decompensated state
-Myocardial dysfunction after cardiac arrest
-Continuous intravenous form for inotropic support to bridge patients with late-stage heart failure, stage D.
-Short-term for those hospitalized patients with severe systolic dysfunction who present with low blood pressure .
-Decompensated congestive heart failure because of the sympathomimetic effects.
-Cold septic shock refractory to fluids and dopamine
Digoxin:
Mechanism of action:
Digoxin has two principal mechanisms of action which are selectively employed depending on the indication: Positive Ionotropic: It increases the force of contraction of the heart by reversibly inhibiting the activity of the myocardial Na-K ATPase pump, an enzyme that controls the movement of ions into the heart.
Efficacy over placebo :
The hemodynamic effects of digoxin in heart failure includes; increase cardiac output, decreased capillary wedge pressure, increased left ventricular ejection fraction (LVEF) [15]. A well-known study such as PROVED was a digoxin withdrawal study which resulted in worsened heart failure and a decrease in LVEF [15]. Another study, the RADIANCE trial which included the role of digoxin in patients who were also taking diuretics and ACE-Inhibitors examined the withdrawal effect on the patients. It was revealed that patient’s conditions deteriorated upon withdrawal of digoxin and there was a decrease in LVEF, increase in heart rate and increase in body weight [16]. Ultimately, the triple therapy of digoxin, ACE-Inhibitor, and diuretic patients had a better outcome in heart failure [16].
Indications:
-Heart failure
-Tachyarrythmias
-Atrial fibrillation
-Atrial flutter
-Paroxysmal atrial tachycardia
Heparin 5000:
Mechanism of action:
Heparin binds to the enzyme inhibitor antithrombin III (AT), causing a conformational change that results in its activation through an increase in the flexibility of its reactive site loop. The activated AT then inactivates thrombin, factor Xa and other proteases
Efficacy over placebo :
When given alone to patients with unstable angina, heparin is effective in preventing acute MI and recurrent angina,135136137 and when used in combination with aspirin, the results of a meta-analysis of 6 small trials suggest that the combination also reduces short-term rates of cardiovascular death and MI by ≈30% over those achieved with aspirin alone.134
"double-blind trial of dose-adjusted IV unfractionated heparin (Class I) in 225 patients with partial stable carotid and vertebrobasilar distribution stroke.7 This trial showed that there was no difference in death at 7 days between patients who were treated with unfractionated heparin (1/112 [0.89%]) and those treated with placebo (2/113 [1.77%]). Functional activity at 7 days, 3 months, and 1 year also was not significantly different between groups. At 6 months, the proportion of patients who were dead or dependent was identical for the group that received unfractionated heparin and the group that avoided heparin (62.9% in each)"
Indications:
-Prophylaxis and treatment of venous thromboembolism and pulmonary embolism
-Atrial fibrillation with embolization;
-Treatment of acute and chronic consumptive coagulopathies (disseminated intravascular coagulation)
-Prevention of clotting in arterial and cardiac surgery
-Heparin is used to prevent acute thrombosis after coronary thrombolysis.
-Heparin represents an effective alternative to warfarin for antithrombotic prophylaxis.
Carvediol:
Mechanism of action:
Carvedilol reversibly binds to beta adrenergic receptors on cardiac myocytes. Inhibition of these receptors prevents a response to the sympathetic nervous system, leading to decreased heart rate and contractility.
Efficacy over placebo :
Carvedilol is a non-selective adrenergic blocker indicated for the chronic therapy of heart failure with reduced ejection fraction (HFrEF), hypertension, and left ventricular dysfunction following myocardial infarction (MI) in clinically stable patients
“Quality of life, which was the primary endpoint, improved similarly in the carvedilol and placebo groups, whereas the global assessment by the physicians and the patient exhibited a better response to carvedilol (P < .05). Hospitalization and mortality rate were too low to evaluate a difference, and exercise time and New York Heart Association classification did not change significantly in response to the drug. Left ventricular ejection fraction rose significantly (+0.09) in the carvedilol group compared with the placebo group (+0.02, P = .004).”
Indication:
-Left ventricular dysfunction
-Hypertension
-Treatment of mild-to-severe heart failure of ischemic or cardiomyopathic origin
Acitrom:
Mechanism of action:
It exerts anticoagulant action by preventing the regeneration of reduced Vit K by interfering with Vit k epoxide reductase.
Efficacy over placebo :
It has been documented that prolonged oral anticoagulation with proper control of INR significantly reduces the risk of cerebral stroke compared to placebo in patients with atrial fibrillation.
"all average monthly INR values were within therapeutic range (2.0-3.0) without differences in the quality of treatment. More than 50% (P = 0.721) as well as >75% (P = 0.714) therapeutic INR values were similar in both groups (Figure 4)."
Dytor:
Mechanism of action:
Dytor(Toresamide) Tablet works by increasing the amount of urine produced. This helps your body get rid of extra water thereby relieving symptoms such as shortness of breath and swelling in your arms, legs, or abdomen. This will help you go about your daily activities more easily and make you more confident about being active.
Efficacy over placebo:
“Torsemide-treated patients had lower blood pressure, and higher creatinine and BUN at baseline compared with placebo. On adjusted analysis, torsemide use was associated with a trend toward lower 30-day mortality or HF hospitalization (OR 0.62, 95% CI: 0.37-1.04; P=0.067).”
Indications:
-Congestive Heart Failure. Indicated for treatment of edema associated with heart failure.
-Chronic Renal Failure. Indicated for treatment of edema associated with renal disease.
-Hepatic Cirrhosis. Indicated for treatment of edema associated with hepatic disease. ...
-Hypertension.
3. What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
ANSWER:
Pathogenesis:
The failing heart is unable to generate forward flow
↓
Pre renal hypo perfusion
↓
Inadequate renal afferent flow
↓
Activates:
-RAAS axis,
-Sympathetic nervous system
-Arginine vasopressin secretion
↓
Leading to fluid retention, increased preload, and worsening pump failure.
↓
Heart failure
This patient has type 4 cardiorenal syndrome.
4. What are the risk factors for atherosclerosis in this patient?
ANSWER:
The probable risk factors which may cause atherosclerosis in this patient include:
a)Old age
b)Diabetes type 2
c)Hypertension
5. Why was the patient asked to get those APTT, INR tests for review?
ANSWER:
-The patient is on UFH therapy. UFH potentiates the activity of antithrombin and covalently neutralises thrombin and activated factor X. Monitoring of this therapy is very essential as this plays a major role in the coagulation and anticoagulation cascade of the body and this has be in check. The aPTT used to be the most commonly used method to monitor the effect of UFH therapy.
-We regularly monitor the INR of people using anticoagulants in order to balance the risk of excessive bleeding (when the INR is too high, meaning that the blood is too thin) against the risk of clotting or thrombosis (when the INR is too low or the blood is too thick).
D)A 67 year old female patient came to the OPD with C/O shortness of breath (SOB) since 1/2 hour.
QUESTIONS:
1. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANSWER:
a) Symptomatology in this patient:
1year ago:
Heart burn like episodes
↓
7 months ago:
Diagnosed with TB
↓
30 minutes ago:
shortness of breath
b) Primary etiology:
-High cholesterol diet
-Diabetes mellitus type 2
-Hypertension
2. What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANSWER:
MET- XL:
Mechanism of action:
Met XL 50mg tablet works by relaxing the blood vessels, thus slowing down the heart rate. By doing this, it reduces the workload on the heart of pumping the blood effectively.Met -XL contains metoprolol which belongs to a group of drugs known as beta blockers. Metoprolol works by blocking the action of certain natural substances in your body, such as epinephrine, on the heart and blood vessels. This effect lowers your heart rate, blood pressure, and strain on your heart.
Efficacy over placebo:
A subgroup analysis of MERIT-HF shows that patients with heart failure and a history of hypertension received a similar benefit from metoprolol CR/XL treatment as all patients included in the total study.
"Treatment with metoprolol CR/XL compared with placebo resulted in a significant reduction in total mortality (relative risk [RR], 0.61; 95% confidence interval [CI], 0.44-0.84; P =.0022), mainly because of reductions in sudden death (RR, 0.51; 95% CI, 0.33-0.79; P =.0022) and mortality from worsening heart failure (RR, 0.49; 95% CI, 0.25-0.99; P =.042). Total number of hospitalizations for worsening heart failure was reduced by 30% in the metoprolol CR/XL group compared with placebo (P =.015). Metoprolol CR/XL was well tolerated: 12% fewer patients withdrew from study medication (all-cause) compared with placebo (P =.048).”
Indications:
-Left ventricular dysfunction
-Hypertension
-Treatment of mild-to-severe heart failure of ischemic or cardiomyopathic origin
-NSTEMI
3. What are the indications and contraindications for PCI?
ANSWER:
Clinical indications for PCI include the following:
-Acute ST-elevation myocardial infarction (STEMI)
-Non–ST-elevation acute coronary syndrome (NSTE-ACS)
-Unstable angina.
-Stable angina.
-Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
-High risk stress test findings.
Clinical contraindications for PCI include:
-Intolerance of long-term antiplatelet therapy
-Presence of any significant comorbid conditions that severely limit the lifespan of the patient (this is a relative contraindication).
-A Heart Team approach (involving interventional cardiologists and cardiac surgeons) should be used in patients with diabetes and multivessel coronary artery disease and in patients with severe left main disease and a high Syntax score.
Relative angiographic contraindications include the following:
-Arteries < 1.5 mm in diameter
-Diffusely diseased saphenous vein grafts
-Other coronary anatomy not amenable to PCI
4. What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on over testing and overtreatment important to current healthcare systems?
ANSWER:
a) What happens if a PCI is performed in a patient who does not need it
The 2013 American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guidelines for the management of STEMI consider primary PCI as a class I indication in STEMI patients within 12 hours’ of initial symptom onset.2 Beyond this timeframe PCI does not show benefit, as shown in the occluded artery trial which evaluated PCI benefit among stable, high-risk patients with persistent total coronary occlusion after MI. The study concluded that PCI performed from 3 to 28 days after MI does not decrease the incidence of death, reinfarction or New York Heart Association (NYHA) class IV heart failure but it is associated with higher rates of both procedure-related and true ST elevation reinfarction.3 A retrospective analysis of the clinical data revealed The Thrombolysis in Myocardial Infarction (TIMI) Risk Score of 4 predicting a 30-day mortality of 7.3% in this patient. Late PCI leads to the increased risks of periprocedural complications, long-term bleeding, and stent thrombosis.
b) What are the harms of overtreatment
Over diagnosis and over treatment are one of the newest treatment difficulties encountered in the management of a patient. The main diffuculty with these new age problems is the diagnosis of an abnormality in the patient and treating it when such diagnosis and treatment does noes help the patient at all and in turn puts the patient to various difficulties such as:
a)Psychological problems: causing unnecessary fear, resulting in increased sense of vulnerability and psychological anguish.
b) Economical problems: The effects of over diagnosis and over treatment will cause the health care not being viable economically to the normal people of the community.
c) why is research on over testing and overtreatment important to current healthcare systems?
There is urgent need of development of evidence-based decision-making tools for clinicians which will help patients understand the benefits and harms of different screening and treatment methods. Eventually the treating physician should be able to convince the patient that watchful waiting, for some of the lesions may be the best option available in some circumstances
E) A 60year old Male patient, came to the OPD with the chief complaint of chest pain , giddiness and profuse sweating .
QUESTIONS:
1. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANSWER:
a) Symptomatology in this patient:
Since 3days:
Chest pain
↓
Since morning:
Giddiness
Profuse sweating
b)Anatomical location of the lesion: inferior wall of the heart.
c)Primary etiology:
-Smoking
-Diabetes mellitus
-Hypertension
2. What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANSWER:
Aspirin:
Mechanism of action:
There are at least two different cyclooxygenase isozymes: COX-1 (PTGS1) and COX-2 (PTGS2). Aspirin is non-selective and irreversibly inhibits both forms(but is weakly more selective for COX-1). It does so by acetylating the hydroxyl of a serine residue. Normally COX produces prostaglandins, most of which are pro-inflammatory, and thromboxanes, which promote clotting. Inhibition of COX-1 results in the inhibition of platelet aggregation for about 7-10 days (average platelet lifespan).Thus helps in relieving the clots formation in the coronary artery during myocardial infarction.
Efficacy over placebo :
Aspirin therapy is well-accepted as an agent for the secondary prevention of cardiovascular events and current guidelines also define a role for aspirin in primary prevention. The body of evidence supports a role for aspirin in both secondary and primary prevention of cardiovascular events in selected population groups
Overall, aspirin significantly reduced the risk of non-fatal MI compared with placebo (RR = 0.72, 95% CI 0.64–0.81, p < 0.001) (Figure 2). There was a trend towards lower fatal MI rates with aspirin (RR = 0.88, 95% CI 0.75–1.03, p = 0.120) (Table 2).
Indications:
-Reducing the risk of cardiovascular death in suspected cases of myocardial infarction
-Reducing the risk of a first non-fatal myocardial infarction in patients, and for reducing morbidity and mortality in cases of unstable angina and in those who have had a prior myocardial infarction
-Reducing the risk of transient ischemic attack
Atorvas:
Mechanism of action:
Actorvas(atorvastatin) is a cholesterol-lowering medication that belongs to the statin class of drugs. Statins lower cholesterol levels in the blood by blocking 3-hydroxy-3methylglutaryl coenzyme A (HMG CoA) reductase, an enzyme that's needed for the liver to produce cholesterol
Efficacy over placebo:
The Effects of Atorvastatin on Early Recurrent Ischemic Events In Acute Coronary Syndromes (MIRACL) trial and the Atorvastatin for Reduction of Myocardial Damage During Angioplasty-Acute Coronary Syndromes (ARMYDA-ACS) trial demonstrated a reduction in mortality rates in patients who received high-potency statins after an episode of Myocardial infarction . High-intensity statin therapy might be beneficial in patients with MI compared to placebo.
Indications:
-Reduce the risk of non-fatal myocardial infarction.
-Reduce the risk of fatal and non-fatal stroke.
-Reduce the risk for revascularization procedures.
-Reduce the risk of hospitalization for CHF.
-Reduce the risk of angina.
Mechanism of action:
The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible.
Efficacy over placebo:
Among patients with ST elevation MI, treatment with clopidogrel was associated with a reduction in mortality and in the composite of death, MI, or stroke compared with placebo.
"The primary endpoint of all-cause mortality by hospital discharge was significantly lower in the clopidogrel group (7.5%, n=1,726 vs. 8.1%, n=1,845; p=0.03). Additionally, the co-primary composite endpoint of death, reinfarction, or stroke was lower in the clopidogrel group (9.2%, n=2,121 vs. 10.1%, n=2,310; p=0.002). Reinfarction was lower in the clopidogrel group (2.1% vs. 2.4%, p=0.02), but stroke did not differ by treatment group (0.9% vs 1.1%, p=NS). Any major bleed occurred in 0.58% of the clopidogrel group and 0.55% of the placebo group"
Indications:
-Use during a percutaneous coronary intervention (PCI) for acute coronary syndrome (ACS) and stable ischemic heart disease.
[4][5][6] -Primary prevention of thromboembolism atrial fibrillation
-STEMI
PTCA:
Efficacy over placebo:
Clinical indications for PCI include the following:
-Acute ST-elevation myocardial infarction (STEMI)
-Non–ST-elevation acute coronary syndrome (NSTE-ACS)
-Unstable angina.
-Stable angina.
-Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
-High risk stress test findings
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
ANSWER:
The patient had already crossed the window period of 12 hours by the time the secondary PTCA was done. After the window period the PTCA has been studied to not show much of a benefit in the patient. The patient was also getting better and was in a steady condition and hence the secondary PTCA was unnecessary.
F) An 87 year old male patient presented to the OPD with chief complaints of shortness of breath, constipation and decreased urine output.
QUESTIONS:
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
ANSWER:
The patient was suffering from hypovolemia which might have been the reason for his shortness of breath. The patient was treated using IV fluids which helped treat the condition
2. What is the rationale of using toresamide in this patient?
ANSWER:
The patient was suffering from dyspnoea due to excess fluid accumulation and congestion inside the body.
Toresamide is a loop diuretic. It works on the kidney and increases the excretion of Na+ and water from the body thereby relieving the patient of his symptoms and also of his hemodynamic irregularities.
This is the rationale of using torsamide in the patient
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
ANSWER:
The patient’s urine test indicates the presence of pus cells in urine which indicates the presence of urinary tract infections (UTI) . The patient was administered ceftriaxone which is an antibiotic commonly used in treatment of pyogenic UTI.
Cefriaxone administration was a treatment therapy and not a prophylactic.
D)GASTROENTEROLOGY & PULMONOLOGY
A)A 33 yr old male daily wage labourer from miryalaguda who is a chronic alcoholic and smoker came to hospital on 30/04/2021 with cheif complaints of pain abdomen & vomiting since 1 week and constipation, burning micturition, fever since 4 days.
QUESTIONS :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer :
a) Evolution of symptomatology :
5years back:
-Patient was apparently asymptomatic
-He developed pain abdomen and vomitings
-Taken to a local hospital and treated conservatively
-Following this he stopped consuming alcohol and was symptom free for the next 3 years
↓
1year back:
-He again started consuming alcohol following which he had recurrent episodes of pain abdomen and vomitings
-He had 5-6 episodes of pain abdomen and vomitings in the last year which were treated by a local RMP
↓
20days back:
-From 20days the patient had consumed increased amounts of alcohol about 5 bottles of toddy per day
-Last binge of alcohol 1 week back following which he again developed pain abdomen and vomitings from 1 week and fever since 4 days
-Burning micturition since 4days associated with suprapubic pain, increased frequency and urgency
↓
Presenting symptoms:
-Pain abdomen and vomitings since 1week
-Fever since 4days
-Abdominal pain localised to hypochondriac, left lumbar and hypogastric regions
-Abdominal pain increased after food intake
-Pain is of throbbing type and radiating to the back and is associated with nausea and vomitings(1episode), which was non bilious, non projectile and also had food particles and water content for 1 week
-Fever was high grade, continuous and not associated with chills and rigors
-Not associated with loose stools
-He developed constipation since 4days and passing flatulus
-Patient also had burning micturition since 4 days
-Burning micturition since 4days associated with suprapubic pain, increased frequency and urgency
b) Anatomical localization of the disease :
•Acute on chronic pancreatitis with pseudocyst & acute infective peri pancreatic fluid collections. The disease is localised to pancreas which lies behind the peritoneum of the posterior abdominal wall and is oblique in its orientation. The head of the pancreas is on the right side and lies within the “C” curve of the duodenum at the second vertebral level
•Moderate left pleural effusion with basal atelectasis with a build-up of fluid between the tissues that line the lungs and the chest
•Left pneumothorax secondary to broncho pleural fistula. This condition occurs when air leaks into the space between the lungs and chest wall.
c) Primary etiology of the patient's problem:
Primary etiology of the patient's main problem that is pancreatitis is due to chronic and excess consumption of alcohol. The pancreatic acinar cells metabolize alcohol into toxic byproducts that damage pancreatic ducts, and enzymes that are normally released into the digestive tract build up and begin to digest the pancreas itself. The damaged pancreatic tissue promotes inflammation, which leads to further damage of the pancreas.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Answer :
a)Efficacy of drugs used along with other non pharmacological treatment modalities :
•Meropenem
Efficacy :
There are few randomized clinical trials about the use of antibiotics in AP. Pederzoli et al. in 1993 [16] conducted the first of them, which analyzed 74 patients with SAP in six medical centers in Italy. The patients were randomized in two groups: one control with 33 patients and the treatment group with 41 patients that received Imipenem 3 × 500 mg/day intravenously (i.v.) during 14 days. They observed reduction in pancreatic sepsis in patients that received antibiotics (30.3% vs. 12.2%, p < 0.01). However, they did not find reduction in mortality between the groups (12% vs. 7%, respectively).
•Inj. Metrogyl 500mg iv TID for 5 days
Efficacy over placebo:
In 2004, the Ulm group in Germany published the best study regarding the use of antibiotics in AP [21]. It was a prospective randomized double-blind trial that analyzed 114 patients, 58 that received antibiotics (Metronidazole 2 × 500 mg/day i.v.) and 56 that received placebo. It was established that if any patient developed systemic inflammatory response, organic failure, any kind of infection or clinical deterioration, this patient would be discontinued from the protocol with open antibiotic treatment. Their results showed that the use of antibiotics did not reduce pancreatic infection (12% antibiotics vs. 9% placebo, p = n.s.) and mortality (5% antibiotics vs. 7% placebo, p = n.s.). However, 28% of patients in the group that received antibiotics had their protocol opened, versus 46% in the placebo group (p = 0.037). Furthermore, the mean time to open the protocol was 11.5 days in the treatment group and 5 days in the placebo group (Table 2). Based on these data, it is reasonable to suppose that a group of patients had benefits receiving early antibiotics.
•ING. AMIKACIN 500 mg IV BD for 5days
Efficacy over placebo:
Gram negative and Gram positive organisms and fungi may have an important role in infective morbidity and mortality in acute pancreatitis, and selective decontamination with antibiotics like amikacin reduced the incidence of translocation related infections and early mortality in patients with acute necrotising pancreatitis.
•TPN ( Total Parenteral Nutrition )
Efficacy over placebo :
The experimental data would thus suggest that use of TPN in patients with acute pancreatitis and pancreatic malignancy might result in some clinical benefit by decreasing activity of the pancreas.
Patients with necrotizing pancreatitis suggests that EN may cause complications in patients with ductular damage. In the second week, the patients with acute pancreatitis and enteral route of food administration developed >50% pancreatic necrosis, resulting in gastroduodenal obstruction and pain, leading to the use of TPN being a safer and a recommended option.
•IV NS / RL at the rate 12l ml per hour
Efficacy over placebo:
Fluid resuscitation has emerged as a key therapeutic strategy in patients with acute pancreatitis. It has to be acknowledged that fluid resuscitation in AP is a complex process, with need to take into account the dynamics of fluid sequestration during different stages of the disease. Current knowledge suggests that controlled fluid resuscitation (3.0-4.0 L/24 h) should be started after a bolus infusion of 20 mL/kg (1000 mL over one hour). Among the different fluids, lactated Ringers’ is the one recommended by most guidelines.
References:
•ING. OCTREOTIDE 100 mg SC , BD
Efficacy over placebo :
The complication rate was lower in the treatment group with regard to sepsis (24% vs 76%, P = 0.0002) and ARDS (28% vs 56%, P = 0.04). The hospital stay was shorter in the treatment group (20.6 vs 33.1 days, P = 0.04). Two patients died in the treatment group and eight in the control group (P < 0.019). These results suggest that octreotide may have a beneficial effect in the treatment of severe acute pancreatitis.
•ING. PANTOP 40 mg IV, OD
Efficacy over placebo :
Histology showed that PPZ treatment reduced tissue infiltration of inflammatory cells and acinar cell necrosis in severe AP. After PPZ treatment CD62P expression in mild AP and CD31 expression in severe pancreatitis decreased, indicating an inhibition of platelet activation. In mild and severe AP, PPZ significantly decreased amylase, LDH, edema and myeloperoxidase activity. Protein profile of pancreatic juice and serum revealed different spectra and less pancreatic juice proteins in PPZ treated groups indicating less acinar cell leakage.
•ING. THIAMINE 100 mg in 100 ml NS IV , TID
Efficacy over placebo :
Thiamine is often recommended to patients with chronic alcoholism to prevent the sideeffects of Wernicke's encephalopathy and other side effects.
•ING. TRAMADOL in 100 ml NS IV , OD
Efficacy over placebo:
Pain intensities (mean ± SD, 0 = none, 100 = unbearable) before treatment andon day 4 were 75 ± 19 and 8 ± 13 withtramadol (P < 0.001), and 65 ± 21 . On day 4, 67%of patients with tramadol rated their analgesia asexcellent (P < 0.001) with mean respective doses of840 mg (range: 80-1920) . Orocecaltransit was unchanged after five days of tramadol. Rectal distension threshold pressures increased with tramadol (P < 0.01). It is concluded tramadol is a potent analgesic in severe chronic pancreatitis pain. Tramadol interfered significantly less with gastrointestinal function and was more often rated as an excellent analgesic.
b) Approach to the case as a treating physician:
B) A 25 year old man,daily wage worker and tractor driver by occupation, presented with severe abdominal pain since 4 days,One episode of vomiting 2 hours before presenting to hospital,Shortness of breath on walking since 2 hours
QUESTIONS :
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
Answer :
The cause of dyspnoes is most probably due to acute pancreatitis in the patient. The mechanism of causing dyspnoea in pancreatitis patient is :
With severe pancreatitis there are a lot of inflammatory chemicals that are secreted into the blood stream. These chemicals create inflammation throughout the body, including the lungs
Two different phases in ALI(Acute lung injury) and ARDS(Acute respiratory distress syndrome) have been described. Initially, an exudative phase during the first days with diffuse alveolar damage, microvascular injury, type I pneumocyte necrosis, and influx of inflammatory cells and fluid to the pulmonary interstitium has been seen, followed by a fibro-proliferative phase during days 3-7, during which type II pneumocyte hyperplasia, proliferation of fibroblasts and lung repair occur[22]. As a consequence of a pronounced and complex systemic net pro-inflammatory response, both endothelial and epithelial injury is involved in ALI and ARDS
Thus ALI and ARDS often lead to shortness of breath and present as dyspnoea.
2)Name possible reasons why the patient has developed a state of hyperglycemia
Answer :
The metabolic response during acute pancreatitis may depend on the one hand on acute stress, which is similar to that seen in other diseases such as sepsis or clinical situations such as surgical interventions, and on the other hand on damage to the Langerhans’s islets related to pancreatic inflammation. Hyperglycemia develops rather often in the early phase of acute pancreatitis, mainly in patients with severe disease [1–3]. This hyperglycemia could thus be the result of a hyperglucagonemia secondary to stress or the result of decreased synthesis and release of insulin secondary to the damage of pancreatic β-cells
Hence the two reasons for a hyperglycemic state are : One is because that sympathetic hyperactivity makes glucagon elevated. Secondary, microcirculation disorder makes pancreas edema, ischemia and necrosis, affecting secretion and excretion of insulin. In severe acute pancreatitis, there may be ketoacidosis
3)What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
Answer:
The patient is a chronic alcoholic and hence he has elevated liver enzymes and abnormal LFT
Alcohol is known to cause Alcoholic fatty liver and alcoholic hepatitis which eventually lead to elevated liver enzymes in the body
Liver enzymes are typically elevated in chronic alcoholics , and tests of liver function may be abnormal. Up to 35% of heavy drinkers develop alcoholic hepatitis, and of these 55% already have cirrhosis. AH can be mild or severe.
No laboratory test is diagnostic of Alcoholic fatty liver. Characteristic ultrasonographic findings include a hyperechoic liver with or without hepatomegaly. Computed tomography (CT) and magnetic resonance imaging (MRI) can readily detect cirrhosis. The biochemical markers for chronic alcohol consumption that have been most commonly studied are serum GGT, AST, ALT, mean corpuscular volume (MCV) and carbohydrate-deficient transferrin (CDT)[82-84]. An AST to ALT ratio over 2 is highly suggestive of ALD.
4) What is the line of treatment in this patient?
Initial treatment :
•Goal directed fluid resuscitation with ringer's lactate solution nutritional support after 72hrs •ERCP in cases of cholangitis or persistent cholestasis
•No role for prophylactic antibiotics maximal supportive care on icu in case of organ failure
Treatment of necrotising pancreatitis:
•Minimally invasive stepup approach in cases of proven or highly suspective of necrotising pancreatitis
•Interventions preferably delayed until phase of walled off necrosis assess for disrupted or disconnected pancreatic duet following necrotising pancreatitis
Prevention of recurrence:
•Presumed idiopathic pancreatitis
-Repeat abdominal ultrasound
-Endoscopic ultrasound.
•Mildbiliary pancreatitis: cholecystectomy during admission
•Severe biliary pancreatitis: cholecystectomy after 6 weeksInitial treatments in the hospital may include:
Treatment of acute pancreatitis in the hospital :
•Fasting. stop oral food for a couple of days in the hospital in order to give the pancreas a chance to recover
Once the inflammation in pancreas is controlled, we may allow consumption of clear liquids and eating bland food.
If your pancreatitis persists and patient still experience pain when eating, recommend a feeding tube to help get nutrition
•Pain medications. Pancreatitis can cause severe pain. Give medications to help control the pain
•Intravenous (IV) fluids. As the body devotes energy and fluids to repairing pancreas, patient may become dehydrated. For this reason, give extra fluids through a vein in your arm during your hospital stay
Once pancreatitis is under control, treat the underlying cause of pancreatitis. Depending on the cause of pancreatitis, treatment may include:
•Procedures to remove bile duct obstructions. Pancreatitis caused by a narrowed or blocked bile duct may require procedures to open or widen the bile duct
A procedure called endoscopic retrograde cholangiopancreatography (ERCP) uses a long tube with a camera on the end to examine pancreas and bile ducts. The tube is passed down the throat, and the camera sends pictures of the digestive system to a monitor
ERCP can aid in diagnosing problems in the bile duct and pancreatic duct and in making repairs. In some people, particularly the elderly, ERCP can also lead to acute pancreatiti
•Gallbladder surgery. If gallstones caused pancreatitis, recommend surgery to remove gallbladder (cholecystectomy
•Pancreas surgery. Surgery may be necessary to drain fluid from the pancreas or to remove diseased tissue
•Treatment for alcohol dependence. Drinking several drinks a day over many years can cause pancreatitis. If this is the cause of pancreatitis, recommend a program for alcohol addiction. Continuing to drink may worsen pancreatitis and lead to serious complications
Additional treatments for chronic pancreatitis:
Depending on the situation, chronic pancreatitis may require additional treatments, including:
•Pain management. Chronic pancreatitis can cause persistent abdominal pain, recommend medications to control your pain and may refer you to a pain specialis
Severe pain may be relieved with options such as endoscopic ultrasound or surgery to block nerves that send pain signals from the pancreas to the brai
•Enzymes to improve digestion. Pancreatic enzyme supplements can help your body break down and process the nutrients in the foods you eat. Pancreatic enzymes are taken with each mea
•Changes to your diet. Refer to a dietitian who can help you plan low-fat meals that are high in nutrients.
References : https://www.mayoclinic.org/diseases-conditions/pancreatitis/diagnosis-treatment/drc-20360233
C) A 45 year old Female patient, came to hospital with chief complaints of Fever since 3 days , Pain abdomen since 2days Decreased Urine Output since 2 days, Abdominal distension since morning
Patient details : https://chennabhavana.blogspot.com/2021/05/general-medicine-case-discussion-1.html
QUESTIONS :
1) what is the most probable diagnosis in this patient?
ANSWER: Hemoperitoneum is the most probable diagnosis in the patient after analysing the history , examination, and all the investigations.
2. What was the cause of her death?
ANSWER:
The most probable conclusion that one can come is that
The patient had lost large amounts of blood into the abdomen
↓
Excess blood loss from the circulation into abdomen
↓
Lead to state of hypovolemic shock
↓
Uncontrolled shock and death may occur
3. Does her NSAID abuse have something to do with her condition? How?
ANSWER:
The patient’s clinical examination indicates that she is suffering from hepatomegaly. People who consume excess NSAID’s often suffer from a condition known as Drug induced hepatitis. This condition might have lead to the hepatomegaly in the patient. Thus NSAID’s may be associated with hepatomegaly in the patient.
5) NEPHROLOGY:
A) A 52 yr old male patient , presented to hospital with Chief Complaints of SOB , burning micturition and fever.
QUESTIONS:
1. What could be the reason for his SOB ?
ANSWER:
The patient is suffering from Acute kidney injury and TURP syndrome. These two conditions might have caused the condition of shortness of breath.
The conditions of Acute kidney fin jury and TURP syndrome cause a buildup of fluids in the lungs leading to the shortness of breath in the patient. This is the mechanism of shortness of breath in the patient.
2. Why does he have intermittent episodes of drowsiness ?
ANSWER:
The patient presented with drowsiness episodes which were intermittent. These episodes are very much correlating with the classical neurological symptoms due to hyponatremia which the patient has.
Neurological symptoms of hyponatremia:
According to European society of Intensive care Medicine:
Serum Na+ less than 110-115meq/L shows neurological symptoms.
-Mild symptoms: Agitation, Confusion, Dizziness, ataxia.
-Serious symptoms: Cerebral edema, increased ICT
3. Why did he complaint of fleshy mass like passage in his urine?
ANSWER: The patient was secreting excess pus cells in his urine which the patient might have confused to be a fleshy mass in the urine. However this may also be due to peripapillary necrosis and papilla sloughing off in the urine giving a mass like passage in the urine
4.What are the complications of TURP that he may have had?
ANSWER: complications caused in the patient post TURP are:
- Electrolyte abnormalities (hyponatremia and creatinine imbalance)
- Urinary bladder infections and injury
-The patient is also suffering from post TURP syndrome(hyponatremia,coma,blindness,cardio respiratory depression)
B) An 8 year old boy was brought to the OPD with the chief complaint of frequent urination.
QUESTIONS:
1. Why is the child excessively hyperactive without much of social etiquettes ?
ANSWER:
The child has a behaviour of excessive hyperactivity, impulsive behaviour, lack of social etiquette. All these features promote the reason to be centered around ADHD syndrome as these clinical features are commonly noticed in the ADHD spectrum
2. Why doesn't the child have the excessive urge of urination at night time ?
ANSWER:
The child is thought to be having a psychosomatic condition and most probably this condition is an Obsessive Compulsive Disorder (OCD) and hence the child does not urinate excessively during the night as he does during the day
3. How would you want to manage the patient to relieve him of his symptoms?
ANSWER:
The child was examined clinically and appropriate required investigations have been done but no findings have been found to be correlating with any kind of renal abnormalities. Hence the renal interventions and unnecessary.
The child has been though to have a psychosomatic condition such as ADHD and OCD and is currently under a psychiatric consult. Hence the best course of action is to reassure and relax the patient along with psychiatric consult until a diagnosis has been reached.
6) INFECTIOUS DISEASE:
A) A 40 year old female came to the OPD with chief complaints of difficulty in swallowing, fever and cough.
QUESTIONS:
1. Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
ANSWER:
The patient has undergone a series of clinical examinations and investigations and the following findings have been declared :
-Hoarseness of voice
-Laryngeal crepitus
-Cough on consumption of food or liquids
-Dysphagia more to solids initially and later to liquids also
-Regurgitation of food
All these findings in the patient are indicative of a tracheo-esophageal fistula.
2. What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
ANSWER: An international meta-analysis showed that TB-associated IRIS occurred in 15.7% of patients who were treated for both HIV and TB . Since the patient is being treted for both HIV and TB there is a greater risk of developing IRIS in her.
Prevention strategies:
-The timing of the start of the ART is crucial in preventing paradoxical IRIS.
-According to a trial that evaluated starting antiretroviral therapy at three points in TB (SAPiT), ART initiation in TB–HIV patients should be decided based on their CD4 cell counts [70]. -If the CD4 counts are <50 cells·mm−3, ART can be started immediately after the initiation of TB treatment.
-If the CD4+ cell counts are ≥50 cells·mm−3, ART can be delayed.
7)INFECTIOUS DISEASE AND HEPATOLOGY:
CASE AND DISCUSSION :
A)A 55 year old male patient who is a palm tree climber by occupation came on 17th April 2021 with the chief complaints of pain abdomen since one week decrease appetite since one week fever since two days
Patient details :
https://kavyasamudrala.blogspot.com/2021/05/liver-abscess.html
QUESTIONS :
1) Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it? What could be the cause in this patient?
Answer :
Yes , chronic consumption of locally made alcohol might have caused the liver abscess in this patient. Liver abscess is commonly caused due to organisms such as amoeba and other infections. Locally made alcohol is an important predisposing factor for both pyogenic and amebic liver abscess due to the alcoholic effects on the liver
From our study it was undoubtedly proved that alcoholism, mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver. It is also proven that Alcoholism is never an etiological factor for the formation of liver abscess
References : https://www.msjonline.org/index.php/ijrms/article/view/2414#:~:text=Conclusion%3AFrom%20our%20study%20it,of%20alcohol%20over%20the%20Liver.
2) What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
Answer :
A close relationship between the consumption of indigenously brewed alcohol beverages and the occurrence of ALA in the tropics has been established over a period of time by several large-population studies
Reasons for this association between local alcohol beverages and ALA could be multifactorial. Factors influencing the association could be related to the pathogen, contents of beverages, status of the liver, and the immunity of the host. They are more vulnerable perhaps due to the large infective dose of Entamoeba histolytica and other bacterial pathogens ingested with the unhygienically brewed beverage. Associated nutritional status of the population and poor sanitation could also play a pivotal role. Alcohol-induced hepatic dysfunction and possible suppression of amoebistatic immune mechanisms by substances in the beverages could also be attributed in the mechanism [6].
"Alcohol can predispose to ALA through a multitude of mechanisms, including hepatic damage by alcohol, lowered body resistance and suppression of liver function due to poor nutritional status of habitual consumers of alcohol, increased presence of amoebae in the liquor prepared locally with poor regard to aseptic procedures, and depression of immune mechanisms in chronic alcoholics.” A study conducted in India in 2011 [4] showed that 67.5% of patients with amoebic liver abscess are from the low socioeconomic class and 72% were alcoholics. It was also noted that alcoholics had larger abscesses, a greater frequency of complications, and delayed resolution of the abscesses.
All these predisposing factors lead to the causation of pyogenic liver abscess due to amebic infection and other infections of the liver.
References : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6077556/
3) Is liver abscess more common in right lobe ?
Answer :
The usual pattern of abscess formation is that there is leakage from the bowel in the abdomen that travels to the liver through the portal vein. Many cases have an infected biliary tract that causes an abscess via direct contact.
50% of solitary liver abscesses occur in the right lobe of the liver (a more significant part with more blood supply), less commonly in the left liver lobe or caudate lobe.
4) What are the indications for ultrasound guided aspiration of liver abscess ?
Answer :
USG guided aspiration of liver abscess is required in:
•Large liver abscess
•Those patients who appear to be superinfected
•Large abscesses impending rupture/ compression signs
•Thin rim of liver tissue around the abscess
•Sero negative abscess
•Failure in treatment following non invasive treatment for 4-5 days
B) A 21 yr old male student,resident of nakrekal, came to the hospital with the chief complaints of abdominal pain since 20 days and fever since 18 days
Patient details : https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-liver-abcess.html
QUESTIONS :
1. Cause of liver abcess in this patient ?
ANSWER:
The patient is a chronic consumer of locally brewed toddy. Locally brewed toddy has been known to contain various types of infective organisms such as amoebae which commonly infect the liver. Hence people who consume locally brewed toddy are at an increased risk of contracting infections of the liver which may lead to a liver abscess.
Hence the main cause of liver abscess in the patient is most probably due to chronic consumption of locally brewed toddy and alcohol.
2. How do you approach this patient ?
ANSWER:
3. Why do we treat here ; both amoebic and pyogenic liver abcess?
ANSWER:
According to the given case history and presentation of the symptoms, the clinical findings and investigations, it is most probably an amoebic liver abscess. However as the pyogenic liver abscess is also very common treatment therapy against both types of abscesses is administered.
4. Is there a way to confirmthe definitive diagnosis in this patient?
ANSWER:
Diagnosis of pyogenic liver abscess:
- Abdominal USG(ultrasound) is performed to know the location of the abscess
- CT scan is performed along with a contrast and a dye which helps in confirming the location and size of the abscess
- Blood report is performed usually to confirm about elevated WBC’s which are indicative of an ongoing inflammation
8) INFECTIOUS DISEASES (MUCORMYCOSIS, OPHTHALMOLOGY, OTORHINOLARYNGOLOGY, NEUROLOGY)
CASE AND DISCUSSION :
A) 50/Male who is a resident of choutuppal daily wage labourer by occupation came with cheif complaints of fever since 10 days facial puffiness and periorbital edema since 4 days, weakness of right upper limb and lower limb since 4 days, altered sensorium since 2 days
Patient details : http://manikaraovinay.blogspot.com/2021/05/50male-came-in-altered-sensorium.html
QUESTIONS:
1)What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer :
a) Evolution of symptomatology:
3 years back:
-Apparently asymptomatic
-Went to hospital for a regular checkup where he was diagnosed with hypertension
-He was on regular therapy for hypertension
↓
On 18/04/21:
-Went to a local PHC for COVID vaccination
-Since that night he complained of fevers, chills and rigors, low grade fever, no diurnal variation
-It was relieved on medication
-No cough or cold
-Following this the patient had similar complaints for the next three days
-It did not subside on medication (antipyretic)
-Not taken any medication such as steroids,oxygen therapy or antivirals
↓
On 24/04/21:
-Generalised weakness, facial puffiness and periorbital edema
-Patient was in a drowsy state
↓
On 04/05/21:
-Patient presented to the casualty in a altered state with facial puffiness and periorbital edema
-Patient also had weakness of upper and lower limbs
b)Anatomical localisation of the problem:
The patient mainly presented with facial puffiness and periorbital edema localised to the medial eye canthus of the right eye. The patient also had extreme weakness of upper and lower limb. He also complained of generalised weakness of the whole body and altered/drowsy mental state
c)Primary etiology of the patient’s problem:
The pati was in an immunocompromised state due to his chronic undiagnosed diabetes mellitus of type 2. Hence this caused him to develop mucormycosis leading to the disease.
The patient also had a chronic hypertension due to which there was a cerbrovascular attack leading to an infarct in his left temporal and frontal lobes.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Answer :
a)The pharmacological modalities used are
• Itraconazole :
Efficacy over placebo:
Itraconazole is the only marketed azole drug that has in vitro activity against Mucorales There are case reports of successful therapy with itraconazole alone. However, itraconazole prophylaxis has been described as a risk factor for breakthrough mucormycosis. Furthermore, animal studies revealed that itraconazole was completely ineffective against Rhizopus and Mucor spp. even though the isolates were susceptible in vitro . In contrast, itraconazole did have activity in vivo against a hypersusceptible strain of Absidia. Therefore, itraconazole should not be considered a first-line agent against mucormycosis, but its use may be considered as adjunctive therapy in selected situations where highly susceptible fungi have been cultured.
b)Approach as a physician:
Approach to treatment —
Treatment of mucormycosis involves a combination of surgical debridement of involved tissues and antifungal therapy [2,28]. Elimination of predisposing factors for infection, such as hyperglycemia, metabolic acidosis, deferoxamine administration, immunosuppressive drugs, and neutropenia, is also critical. Due to the difficulties in establishing a definitive diagnosis, many patients will be empirically treated for mucormycosis because they have risk factors for infection and positive cultures and/or compatible clinical syndromes.
Intravenous (IV) amphotericin B (lipid formulation) is the drug of choice for initial therapy [108,109]. Posaconazole or isavuconazole is used as step-down therapy for patients who have responded to amphotericin B. Posaconazole or isavuconazole can also be used as salvage therapy for patients who don't respond to or cannot tolerate amphotericin B; for salvage therapy, the decision to use oral or IV posaconazole or isavuconazole depends on how ill the patient is, whether an initial course of amphotericin B was able to be administered, and whether the patient has a functioning gastrointestinal (GI) tract.
Surgery — Aggressive surgical debridement of involved tissues should be considered as soon as the diagnosis of any form of mucormycosis is suspected. Surgical intervention with removal of necrotic tissue and debulking infection has been associated with improved survival in anecdotal clinical reviews of rhinocerebral and pulmonary infection [110,111. In the case of rhinocerebral infection, debridement to remove all necrotic tissue can often be disfiguring, requiring removal of the palate, nasal cartilage, and the orbit.
Antifungal drugs — Early initiation of antifungal therapy improves the outcome of infection with mucormycosis. This was illustrated in a retrospective study of 70 patients with hematologic malignancy who had mucormycosis in which delayed amphotericin B therapy (starting treatment ≥6 days after diagnosis) resulted in an almost twofold increase in mortality at 12 weeks after diagnosis (83 versus 49 percent)
Salvage therapy — We use posaconazole or isavuconazole as salvage therapy for patients who do not respond to or cannot tolerate amphotericin B
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
Answer:
India is has a high number of diabetics and other immunocompromised patients. During recent times and also in covid settings the indiscriminate and non judicious use of steroids has increased the number of immunocompromised individuals in the community. This has lead to the vast and sudden increase in the mucormycosis condition in the community which was not a notified disease in the country.
This is the main reason for the sudden spike in the cases of mucormycosis in india.
9) INFECTIOUS DISEASES (COVID - 19)
The master chart for all the COVID cases in the ward :
https://1drv.ms/x/s!AmWeIn6O65tPgkgzeue3a0JB2MgG
https://1drv.ms/x/s!AmWeIn6O65tPgkWi9mzcvP3VNu94
10) MEDICAL EDUCATION :
Reflective logging of the experience:
The experience gained from the online tele medical log book maintenance and research on various cases has been very interesting and enthralling. For a third year student who has never been exposed to in depth analysis and correlations of various systems in the body in the view of patient treatment has been an amazing experience.
Studying and analysing every case of the log and understanding the context and correlations between different systems and the treatment modalities being applied in a hospital was necessary to understand the different cases. The various intriguing questions asked by the students making the case sheet and E logs has instilled newer approach in viewing and understanding the cases.
Normally due to the busy day schedule during the college hours would have taken away major chunk of time leading to less time and energy to find out in depth regarding the cases and the condition by the student. But due to the covid pandemic and excess time on our hands we have been able to devote our complete time and energy into understanding the cases.
However even though this was a good experience the proper way in which one would want to study a case would be by going to the ward and interacting with the patient, performing all the physical tests and clinical examinations and getting a hands on experience of treating a patient. But keeping the present times in mind the maximum one can do is to study and become thorough with the theoretical aspects of the various cases so that when we go back to the hospital the theoretical knowledge is put to a test by practical experience gained in the wards.
I would like to thank Dr. Rakesh biswas sir for this opportunity which has taught us many things regarding the subject and also intrigued us into finding out various articles and studies which support the text in the books.
I would also like to thank all the Pg's who have taken time from their busy schedule to give us appropriate information regarding the cases and also for their help in clearing all our doubts regarding the cases and their pathologies.





























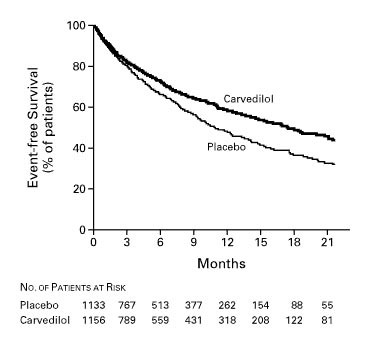










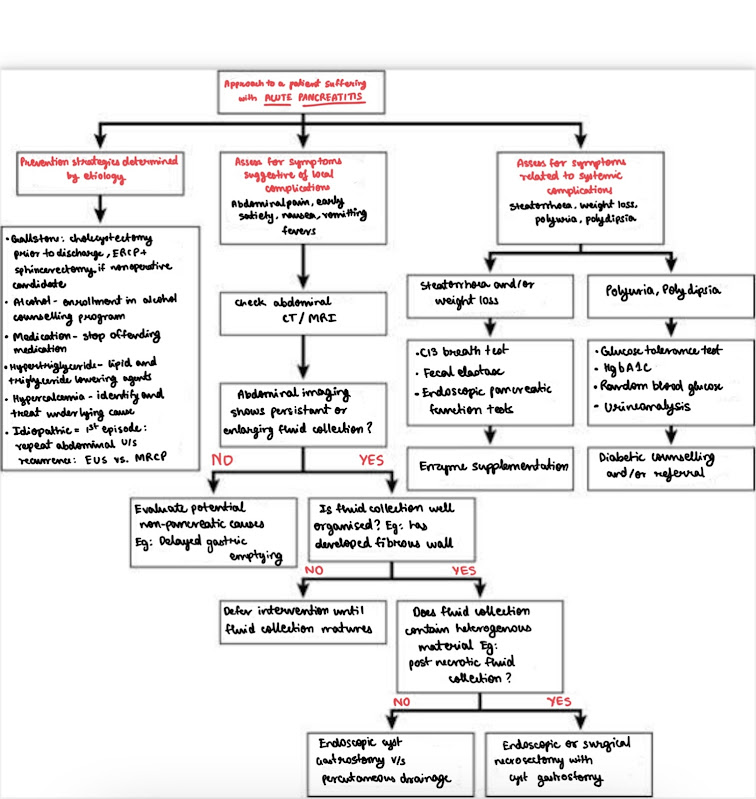














Comments
Post a Comment