42 year old male patient with yellowish discoloration of eyes and skin
42 year old male patient with yellowish discoloration of eyes and skin
18 February 2023
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
42 year old male patient with yellowish discoloration of eyes and skin
Dr. M. Anurag ( Intern )
Roll no : 84
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
CASE :
42 year old male patient was brought to the casuality with chief complaints of
1. Yellowish discolouration of eyes since 1 month
2. Yellowish discolouration of skin since 10 days
HOPI :
Patient was apparently normal 1 month back then he yellowish discolouration of eyes which was insidious in onset, gradually progressive.
Patient also has complaints of yellowish discolouration of skin since 10 days for which he was taken to a local hospital and was treated there.
Patient was unable to do his works from then and was lying on the bed and was not able to do his own works.
Patient also has complaints of vomitings since 4 days which was non projectile, non foul smelling with food particles as contents, non blood stained.
Patient complained of abdominal distention and pain abdomen since 1 day for which he was taken to a local hospital and referred here from there.
There is history of loss of appetite , decreased urine output and high coloured urine. Stools are pale in colour and not passed today ( passed yesterday 2-3 episodes ).
Pedal edema is present but no facial puffiness.
PAST HISTORY :
Not a k/c/o DM, HTN , TB ,epilepsy, asthma,CAD,CVD.
H/O Splenectomy done in 2014 after a Road Traffic Accident. Also operated for fracture of radius and ulna of left arm.
Patient was given Pneumococcal and Hib vaccines after Splenectomy
Patient was started on Tab. Librium 50mg BD after visiting a local hospital 10days back
PERSONAL HISTORY:
Appetite- Decreased since 1 month
Diet - mixed
Bowel - regular
Bladder - Decreased urine output and high coloured urine since 1 month
Addictions -
1. Chronic alcoholic consuming 180ml everyday since 20 years
2. Chewable tobacco consumption since 20 years
FAMILY HISTORY:
No significant family history
GENERAL EXAMINATION:
Pt is C,C,C
Icterus is present .
No pallor, cyanosis, clubbing, lymphadenopathy , pedal edema
Vitals -
Temp -98.6F
PR - 106bpm
BP - 110/80 mmhg
RR - 18cpm
SpO2 - 96% at Room air
Grbs - 129
SYSTEMIC EXAMINATION :
PER ABDOMEN :
Inspection :
Umbilicus is central and inverted
All quadrants are moving equally with respiration
Vertical Scar present over the abdomen.
No sinuses , engorged veins, visible pulsations .
Hernial orifices are free.
Palpitation :
Abdomen is firm in consistency.
Suprapubic bulge till umbilicus is present.
No organomegaly.
Liver - Not palpable
Spleen - Splenectomy done in 2014 in KIMS,NKP
Percussion : Tympanic note heard over the abdomen.
Auscultation:
Bowel sounds are heard.
CARDIOVASCULAR SYSTEM:
Inspection:
Shape of chest is elliptical.
No raised JVP
No visible pulsations, scars , sinuses , engorged veins.
Palpitation:
Apex beat - felt at left 5th intercostal space
No thrills and parasternal heaves
Auscultation :
S1 and S2 heard.
RESPIRATORY SYSTEM:
Inspection:
Shape- elliptical
B/L symmetrical ,
Both sides moving equally with respiration .
No scars, sinuses, engorged veins, pulsations
Palpation:
Trachea - central
Expansion of chest is symmetrical.
Vocal fremitus - normal
Percussion: resonant bilaterally
Auscultation:
bilateral air entry present. Normal vesicular breath sounds heard.
CENTRAL NERVOUS SYSTEM:
Conscious,coherent and cooperative
Speech- normal
No signs of meningeal irritation.
Cranial nerves- intact
Sensory system- normal
Motor system:
Tone- normal
Power- bilaterally 5/5
Reflexes Right Left
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee ++ ++
Ankle ++ ++
INVESTIGATIONS:
CBP:
Hb - 8.3 gm/dl
TLC - 18800 cells/ cumm
RBC - 2.24 million
PLT - 3.45 lakh
RFT:
urea - 16 mg/dl
Creatinine - 0.6 mg/dl
Na - 137 mEq/L
K - 3.6 mEq/L
Cl - 101 mEq/L
LFT :
TB- 11.96 mg/dl
DB- 10.62 mg/dl
SGPT - 13 IU/L
SGOT - 40 IU/L
ALP - 394 IU/L
TP - 6.9
albumin - 2.5 gm/dl
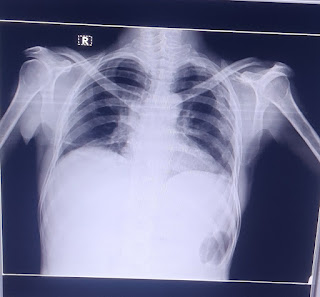
Chest X ray :
ECG :
PROVISIONAL DIAGNOSIS:
DIRECT HYPERBILIRUBINEMIA SECONDARY TO CLD WITH MEGALOBLASTIC ANEMIA SECONDARY TO ALCOHOL
TREATMENT:
1. Salt restriction < 2gm /day
2. Fluid restriction < 1.5 litres/day
3. Inj. Thiamine 200mg IV TID in 100ml NS
4. Inj. Optineuron 1 amp in 100ml NS
5. Tab. Udiliv 300mg PO BD
6. Syr. Lactulose 15ml PO OD H/S
7. Abdominal Girth monitoring
8. Weight monitoring
9. Inj. Vit K 10mg slow OD
10. Inj. Vit B 12 1000 mcg IM OD
11. Tab. Folic Acid 5mg PO OD








Comments
Post a Comment