19 year old male patient with vomitings and shortness of breath
M.Anurag
Roll no 72
MBBS - 4rth year
Roll no 72
MBBS - 4rth year
This is a case of a 19 year old male who presented to the OPD with complaints of vomitings and shortness of breath
This is an online E-Log book to discuss our patient's de-identified data shared after taking his/her/Guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve these patient's clinical problems with collective current best evidence-based inputs. This E-log also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box are welcome.
A 19Y old male, resident of Miryalguda studying degree first year came to the OPD on 24th March 2022 with chief complaints of:
- Vomitings since 2 days
- Shortness of breath since afternoon on 24th March 2022.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic one and half year ago, then he developed polyuria, nocturia, polydypsia and was diagnosed as Diabetic type 1 MISC post COVID and during the hospital stay, on day 5 he went to coma for 7 days, then recovered and discharged after 20 days.
About 4 months ago, he developed vomitings, which was non projectile type , food and water as content, DKA 2° to DM
On 24th March, he presented with 10 episodes of vomitings in 2days, associated with nausea and abdominal discomfort,chest pains, breathlessness after episode of vomiting, non projectile, non bilious and had food particles as contents, not blood stained.Later on the second day he also had an episode of blood tinged vomiting due to which he came to the OPD
H/o outside food consumption.
Shortness of breath at rest, insidious in onset since afternoon,24/03/2022
No aggrevating and relieving factors.
No h/o fever, loose stools, cough and cold, pain abdomen, burning micturition.
PAST HISTORY:
The patient has similar complaints in the past
The patient has a history of diabetes type 1 which was diagnosed last year. No history of Hypertension, Asthma, Tuberculosis.
FAMILY HISTORY:
Insignificant
PERSONAL HISTORY:
Daily routine
- 8am - wakes up
- 9am- breakfast
- 10am to 1pm goes to college
- 2pm- Lunch
- 3pm to 6pm- goes out with friends
- 8 pm- dinner
- 9pm- sleep
- Also works at a petrol pump as a part time job on alternate days for 24 hour shifts
- Diet: Mixed
- Appetite: adequate
- Sleep: adequate
- Bowel and bladder: regular
- No Addictions and allergies
- No surgical history
- Treatment history: INSULIN 52-26-52
GENERAL EXAMINATION:
The patient was examined in a well-lit room after informed consent was taken.
He is conscious, coherent, cooperative, well oriented to time, place and person. He was well nourished and well built.
Weight: 75 kgs
Height: 167cms
BMI: 27.7
No Pallor, Icterus, Clubbing, Cyanosis, Koilonychia, Lymphadenopathy, Edema.
VITALS:
- Temperature: afebrile
- PR: 76bpm
- RR: 18cpm
- BP: 120/80 mmHg
- SpO2: 96% on RA
- GRBS: 157mgdL on 28/03/2022
SYSTEMIC EXAMINATION:
PER ABDOMEN
- Inspection:
- Shape of abdomen - distended
- Umbilicus- transverse slit
- Abdominal movements- equal in all quadrants with respiration, no visible peristalsis.
- Skin- normal, no scars and sinuses, no engorged veins.
- Light palpation- all quadrants are normal, no pain
- Deep palpation- lipodystrophy felt on right iliac fossa
- LIVER: not enlarged
- SPLEEN- not enlarged
- KIDNEYS - bimodal palpable kidneys
- Percussion: no shifting dullness.
- Auscultation: Bowel sounds are heard and are normal.No bruit
CVS: S1 and S2 heard, no murmurs
CNS: NADRS: BAE+
INVESTIGATIONS:
SERUM ELECTROLYTES
Diabetic ketoacidosis 2° to ? inadequate insulin, ?Acute Gastroenteritis.
TREATMENT:
28/03/2022
- IVF - 20 NS, 20 RL @ 100ml / hr
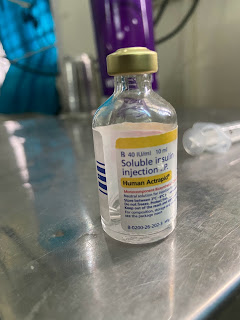
- Inj. HUMAN ACTRAPID 40U in 39ml NS @ 5 ml /hr
- Inj. PANTOP 40 mg IV OD
- Inj. MONOCEF 1gm IV BD
- Inj. ZOFER 4mg IV BD
- INJ. NEOMOL 1 gm IV SOS ( if temp > 101 F)
- Tab. DOLO 650 mg PO SOS
- Inj. 5% dextrose 50 ml / hr ( if GRBS< 250)
- Strict GRBS, BP charting
.png)



.png)














Comments
Post a Comment